Understanding Anatomy Lab Occupancy and Ventilation Requirements
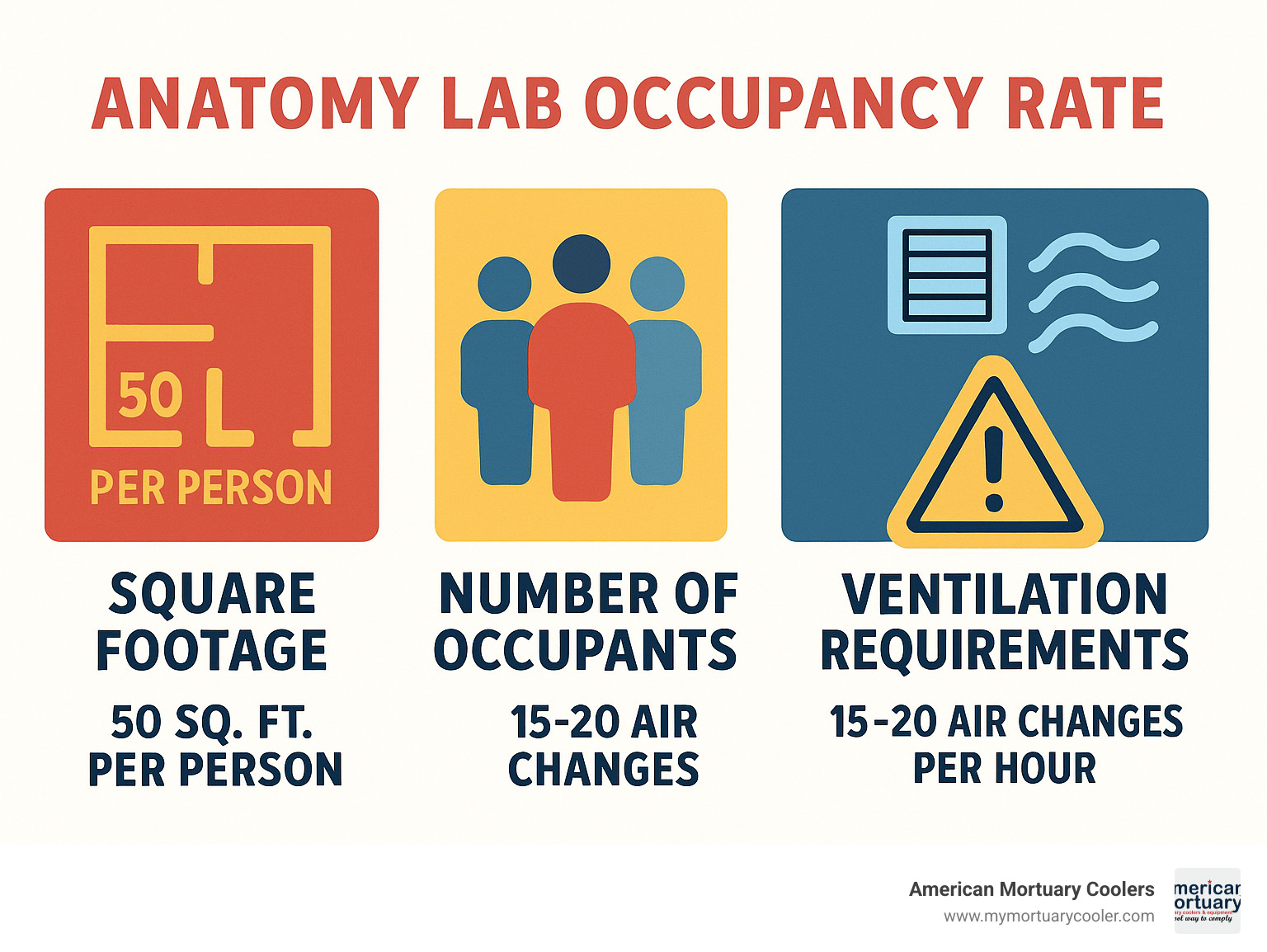
Anatomy lab occupancy rate is the number of occupants per square foot in an anatomy laboratory, typically calculated at 1 person per 50 net square feet according to NFPA standards. Proper occupancy rates ensure safety, compliance with ventilation requirements (15-20 air changes per hour), and effective teaching environments.
The anatomy lab occupancy rate is a critical metric that impacts safety, ventilation requirements, and educational effectiveness in gross anatomy and dissection laboratories. As specialized teaching environments that handle preserved cadavers and chemicals like formaldehyde, anatomy labs must balance space utilization with strict safety protocols that differ significantly from standard classrooms or even other laboratory types.
When designing or operating an anatomy lab, understanding proper occupancy rates is essential for:
- Safety compliance - preventing overcrowding that could hamper emergency evacuation
- Exposure control - ensuring adequate ventilation for all occupants
- Educational effectiveness - maintaining appropriate student-to-cadaver ratios
- Energy efficiency - balancing ventilation requirements with operational costs
The National Fire Protection Association (NFPA) and other regulatory bodies typically specify that anatomy laboratories should maintain an occupancy rate of 1 person per 50 net square feet, compared to standard classrooms that allow 1 person per 20 square feet. This lower density reflects the specialized equipment, ventilation needs, and circulation space required around dissection tables.
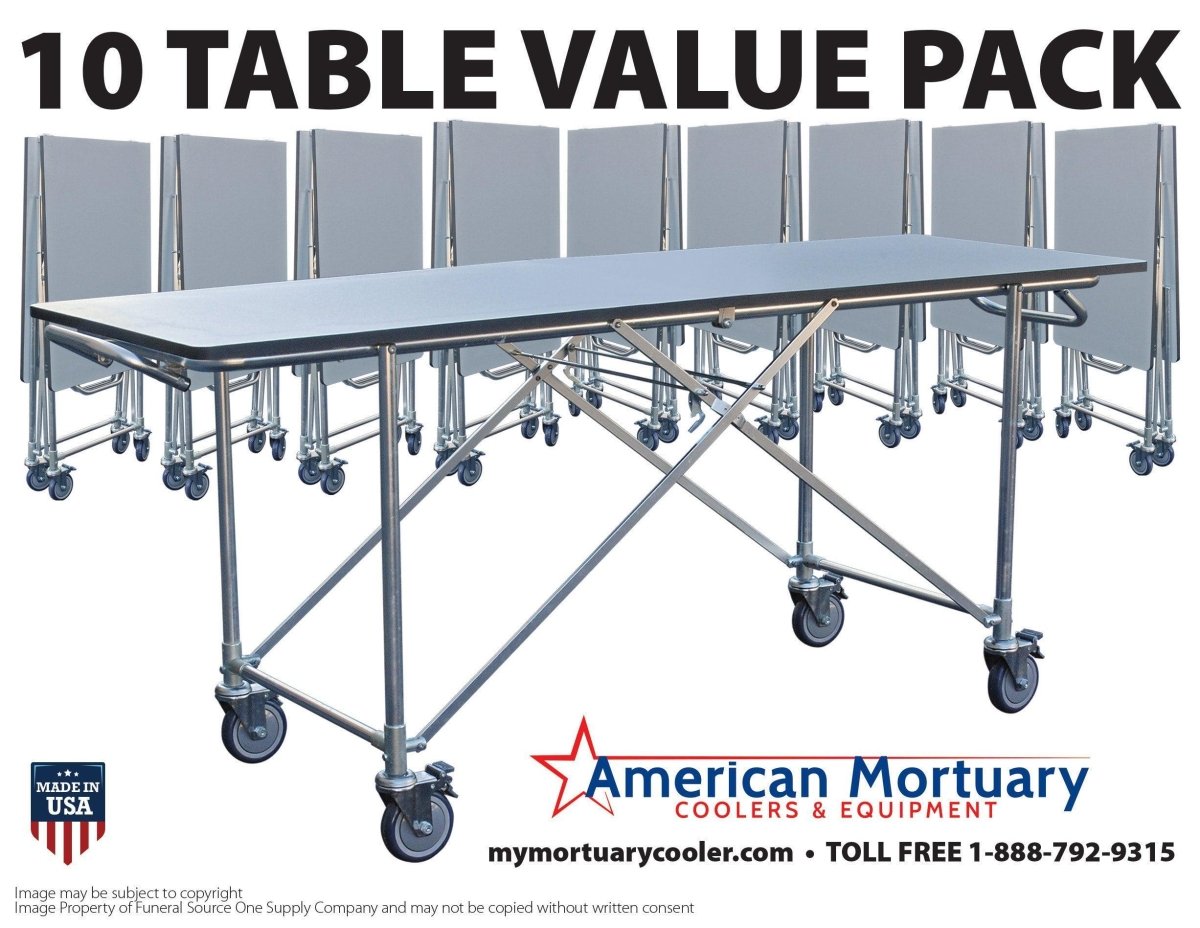
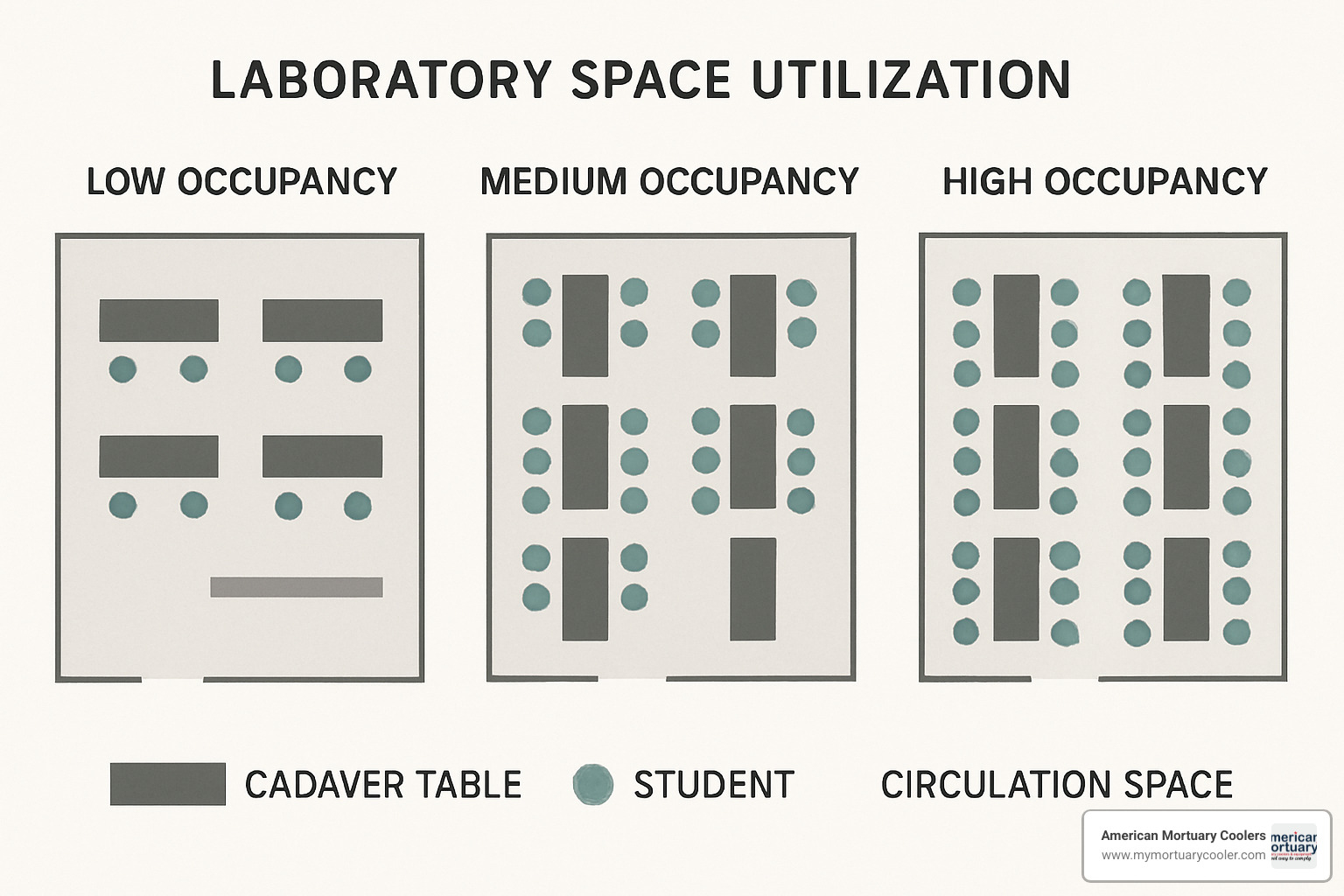
Dissection tables themselves require significant clearance - typically 60 inches head and toe and 40-50 inches to each side - which directly limits the maximum occupancy based on available floor space. A typical gross anatomy lab might accommodate 40-48 students working at 10-12 dissection tables, with ventilation systems designed to provide 15-20 air changes per hour to maintain safe formaldehyde levels below OSHA's permissible exposure limit of 0.75 ppm.
I'm Mortuary Cooler, and I've spent over 15 years designing ventilation and refrigeration systems for anatomy labs where understanding anatomy lab occupancy rate is crucial for maintaining proper air quality and temperature control in these specialized environments. My experience has shown that proper occupancy planning is the foundation for all other safety and operational systems in these facilities.
Find more about anatomy lab occupancy rate:
Anatomy Lab Occupancy Rate: Definition, Significance, and Key Metrics
When we talk about anatomy lab occupancy rate, we're referring to how many people can safely occupy an anatomy laboratory at one time. This isn't just about cramming in as many students as possible – it's about creating a space that's safe, functional, and conducive to learning.
Unlike regular classrooms where students might sit shoulder-to-shoulder, anatomy labs need breathing room – literally and figuratively! The standard recommendation is 50 net square feet per person, which is more than double what's required for a typical classroom. This extra space accommodates the specialized equipment and ensures everyone can move safely around cadaver tables.
Speaking of cadaver tables, they need plenty of clearance – typically 60 inches at the head and foot and 40-50 inches on each side. This spacing isn't arbitrary; it allows instructors to circulate, students to observe without crowding, and provides quick access in case of emergency.
When planning an anatomy lab, we also look at utilization hours – most educational standards recommend at least 18 hours of scheduled use per week to justify the significant investment these specialized spaces require. This helps institutions balance their resources while ensuring students get the lab time they need.
"Adhering to legal occupancy standards isn't optional," as laboratory safety expert Dr. Ken Roy often emphasizes. "It's essential for safe, lawful operation of anatomy laboratories." Exceeding design capacity isn't just uncomfortable – it creates health risks and potential legal liability.
What Is "anatomy lab occupancy rate" and How Is It Calculated?
The anatomy lab occupancy rate can be calculated in several practical ways:
Most commonly, we use the net square footage method:
Occupancy Rate = Total Net Square Footage ÷ 50 square feet per person
For example, if you have a 1,250 square foot anatomy lab, your maximum occupancy would be 25 people. Simple enough!
When working with gross square footage (which includes walls and corridors), we adjust our calculation:
Occupancy Rate = Total Gross Square Footage ÷ 65-70 square feet per person
Many anatomy departments prefer a more practical approach based on their teaching setup:
Maximum Occupancy = (Number of Tables × Students per Table) + Instructors
UC Riverside's Gross Anatomy Suite, for instance, planned around 12 tables with 4 students per table, creating space for 48 students plus their instructors.
It's worth noting that "net square feet" refers to the actual usable floor space. This excludes walls, columns, and fixed equipment – it's the measurement that matters most for safety regulations and building codes.
Why Does Anatomy Lab Occupancy Rate Matter for Education and Safety?
The anatomy lab occupancy rate isn't just a number – it directly affects both learning outcomes and safety.
From a safety perspective, proper occupancy planning prevents several serious issues. First, it helps control exposure to chemicals like formaldehyde. As one experienced lab manager told the ASCP Vacancy Survey, "We cannot exceed our ventilation capacity without risking exposure to harmful chemicals." With preserved specimens in the room, proper air flow for each person is non-negotiable.
Proper occupancy planning also ensures everyone can exit quickly in an emergency. NFPA standards require labs with hazardous materials that are larger than 200 square feet to have two exits – but those exits won't help if the lab is so crowded that people can't reach them quickly.
The space between tables also prevents accidents. When students have room to move, they're less likely to bump into each other or equipment, reducing the risk of spills or injuries. NC State University's Design Guidelines highlight the importance of "separation from non-lab spaces with dedicated storage and circulation corridors" for this very reason.
On the education side, the right anatomy lab occupancy rate ensures everyone gets hands-on experience. Most anatomy programs aim for 4-6 students per cadaver table – enough to share the workload while ensuring everyone can participate meaningfully. With too many students, some inevitably become spectators rather than participants.
Faculty need space to teach effectively too. A typical ratio includes one teaching assistant per 12-16 students, and these instructors need room to move between tables, demonstrate techniques, and supervise students' work.
As one faculty member noted in the UCR Gross Anatomy Suite Study, "We need to design for up to 48 students with infrastructure for expansion, even if initial use is for 40." This forward-thinking approach recognizes that good occupancy planning creates flexibility for the future while ensuring safety and learning effectiveness today.
Benchmarking & Comparative Analysis Across Lab Types
Ever wonder how your anatomy lab stacks up against others? You're not alone! When planning or evaluating anatomy laboratories, comparing occupancy rates across different lab types gives you valuable context to ensure your space meets both industry standards and your specific needs.
I've spent years helping universities optimize their specialty lab spaces, and I've found that benchmarking is one of the most eye-opening exercises for lab managers. The State Council of Higher Education for Virginia (SCHEV) provides some really helpful utilization guidelines that serve as good starting points:
Class laboratories should aim for at least 18 hours of use per week per station. That's roughly equivalent to scheduling the space for 24 weekly hours with a 75% fill rate.
General classrooms, by comparison, target at least 24 hours per week per station (about 40 weekly hours scheduled with 60% fill).
Notice the difference? Specialized laboratories like anatomy labs typically have lower utilization rates than general classrooms. This makes perfect sense when you consider their specialized nature and the extra setup time required between sessions.
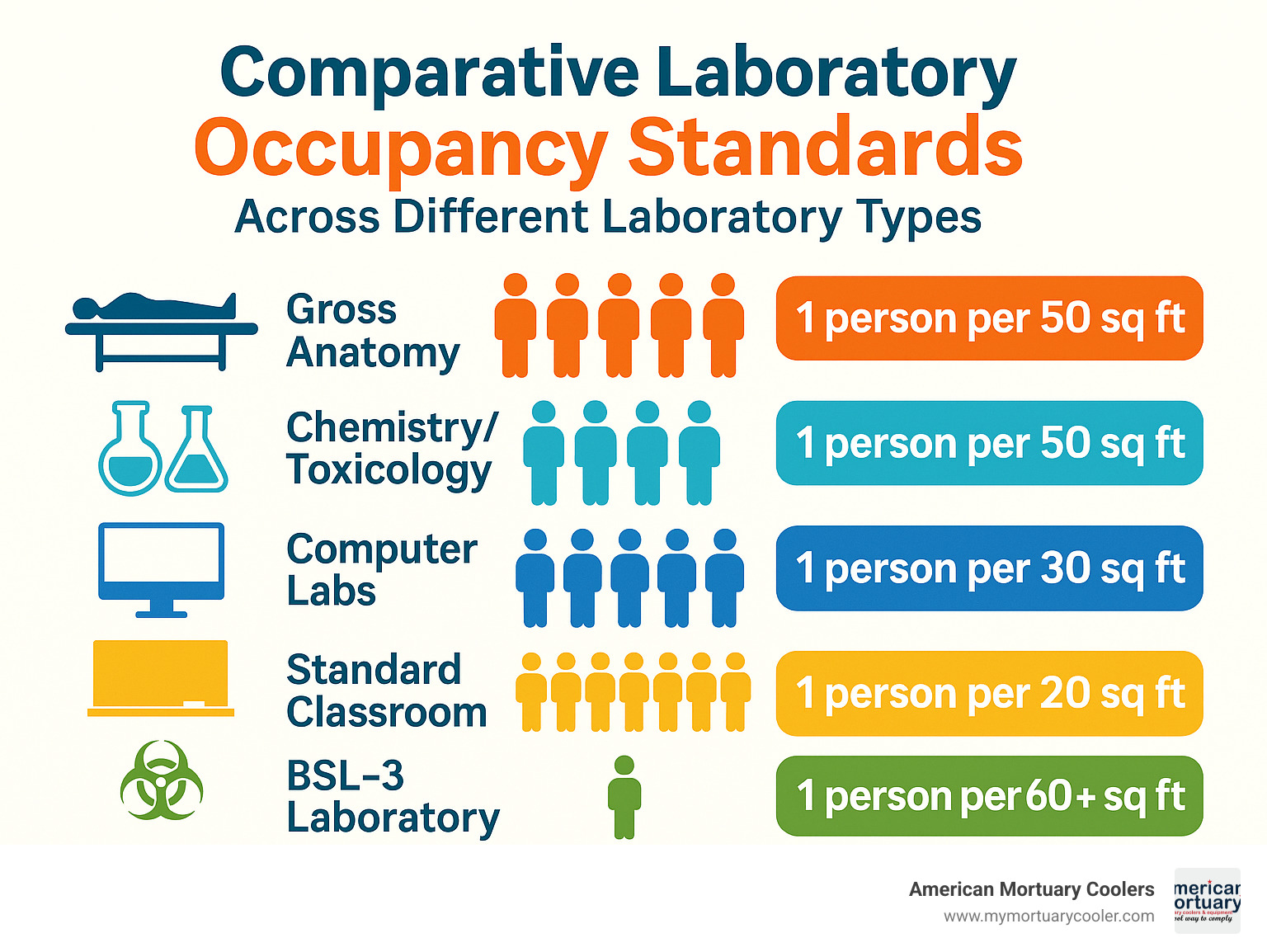
Here's how different lab types typically compare:
| Laboratory Type | Typical Occupancy Rate | Minimum ACH | Space per Person | Weekly Utilization Target |
|---|---|---|---|---|
| Gross Anatomy | 1 person per 50 sq ft | 15-20 ACH | 50-60 sq ft | 18 hours/week |
| Chemistry/Toxicology | 1 person per 50 sq ft | 6-12 ACH | 50 sq ft | 18 hours/week |
| Computer Labs | 1 person per 30 sq ft | 6 ACH | 30 sq ft | 24 hours/week |
| Standard Classroom | 1 person per 20 sq ft | 4-6 ACH | 20 sq ft | 24 hours/week |
| BSL-3 Laboratory | 1 person per 60+ sq ft | 12+ ACH | 60+ sq ft | Variable |
Typical Anatomy Lab Occupancy Numbers at U.S. Universities
Let's peek inside some real-world examples to see how universities are implementing anatomy lab occupancy rate standards in practice:
The University of California, Riverside (UCR) designed their Gross Anatomy Lab with thoughtful attention to detail. They opted for 10-12 dissection tables with 4 students per table, accommodating a maximum of 48 students. The total assignable space comes in at 2,115 ASF, with ventilation cranked up to 20 air changes per hour to ensure safety.
I visited this lab last year and was impressed by how the space flow worked even at full capacity – students had enough room to move around tables without bumping into each other, which is crucial when handling delicate specimens.
North Carolina State University takes a precise approach with their design guidelines. They require dissection tables to have minimum clearances of 60 inches at the head and toe, with side clearances of 40-50 inches between tables. They've also incorporated seamless coves extending eight inches up walls and specified impermeable, smooth finishes throughout – smart choices that make cleanup easier and prevent contamination.
A colleague who manages the NC State facility told me, "These clearances aren't just arbitrary numbers – they're the minimum needed to ensure students can work comfortably while instructors can still circulate and provide guidance."
In my broader research of medical school anatomy labs across the U.S., I've found most institutions design for 40-48 students in first-year gross anatomy courses. Section sizes are typically determined by the number of available cadavers and the educational model, with 4-6 students per cadaver being the sweet spot.
As one anatomy lab director candidly shared with me, "We balanced our occupancy between having enough students to justify the expense of each cadaver while ensuring every student gets hands-on dissection experience. Too many hands on one cadaver and the educational value plummets."
How Do Anatomy Labs Compare with Wet Chem Labs and Computer Labs?
Different laboratory types have distinct occupancy patterns based on their function, equipment, and safety needs. Understanding these differences helps put anatomy lab occupancy rate in context:
When comparing anatomy labs to chemistry labs, several key differences emerge. Both maintain the standard of 1 person per 50 sq ft, but anatomy labs typically require 15-20 air changes per hour compared to chemistry labs' 6-12 ACH. This higher ventilation requirement directly impacts energy costs and mechanical system design.
Chemistry labs also tend to enjoy more flexible scheduling due to easier setup and teardown between classes. An interesting side note: the American Society for Clinical Pathology found chemistry/toxicology departments had the highest vacancy rate (12.7%), which potentially affects utilization rates at many institutions.
The comparison between anatomy labs and computer labs reveals even more striking differences. Real-time data from Lehigh University's LTS Computing Center shows computer labs maintain higher density – approximately 1 person per 30 sq ft. They also achieve higher utilization rates, with some computer labs operating 24/7, and require less ventilation (6 ACH vs. 15-20 ACH).
A former IT director I worked with explained, "Computer labs are basically plug-and-play spaces. Students can walk in, log on, and get to work with virtually no setup time. That's a luxury anatomy labs just don't have."
Virginia Tech's benchmarking data reveals another interesting pattern: class laboratories (including anatomy labs) are expected to maintain 75% fill rates during scheduled hours, compared to 60% for general classrooms. This higher fill rate acknowledges both the specialized nature and higher cost per square foot of laboratory spaces.
The fundamental difference really comes down to purpose: anatomy labs handle biohazardous materials and chemicals requiring specialized ventilation and safety protocols, while computer labs primarily manage electrical and ergonomic concerns. This core difference drives nearly every aspect of design, from space allocation to mechanical systems.
How Occupancy Rate Drives Ventilation Design, ACH, and Energy Use
When you walk into a well-designed anatomy lab, you might notice it doesn't smell like chemicals—that's good ventilation at work! The anatomy lab occupancy rate plays a starring role in how ventilation systems are designed, and ultimately, how much energy the lab consumes.
Think of ventilation as the lab's lungs. Most gross anatomy labs need 15-20 air changes per hour (ACH) when people are present—that's roughly three times what's needed in a regular classroom. Why so much? These robust ventilation rates serve multiple purposes: they dilute formaldehyde vapors, maintain negative pressure (so air flows in, not out), control odors, and provide fresh air for everyone working in the space.
The relationship between people and air is fascinating. As one lab manager told me, "Every additional person in the room is like adding a small heater plus a formaldehyde source." Each person contributes body heat, moisture, and potentially disturbs preservation chemicals during dissection.
Interestingly, a Yale University study found that the sweet spot for clearing airborne contaminants happens between 6-8 ACH, with diminishing returns above 12 ACH. This suggests we might be over-ventilating some labs when they're at lower occupancy. As one facility manager put it, "Running at 20 ACH all the time is like driving with your foot to the floor, even in a school zone."
Linking Anatomy Lab Occupancy Rate to Required Air Change Rates (ACH)
The rules around ventilation get pretty specific when it comes to anatomy lab occupancy rate. It's not just about comfort—it's about safety.
ASHRAE (the folks who write ventilation standards) requires a minimum fresh air rate of 0.18 cubic feet per minute (cfm) per square foot for university labs. For a typical lab with 9-foot ceilings, that's roughly 1.2 air changes per hour just as a starting point. But that's just the baseline—occupants add another layer of requirements.
Let me break it down with a real-world example: For a 1,000 square foot anatomy lab with 12-foot ceilings (12,000 cubic feet total) and 20 students plus instructors, you'd need:
- A baseline of 15 ACH for the lab itself
- Plus additional ventilation for 20 people (at 20 CFM per person = 400 CFM)
- Which adds another 2 ACH to the total
- Bringing your total requirement to 17 ACH
OSHA doesn't mess around with formaldehyde exposure, setting a strict limit of 0.75 parts per million (ppm) as an 8-hour average. Proper ventilation is how labs stay under this limit while maintaining a functional teaching environment.
As one professor told me, "The ventilation system is like an invisible shield between us and the chemicals we work with every day."
Mechanical System Design: Supply, Exhaust, and Local Capture
When it comes to keeping anatomy labs safe, there's more than one way to move air. Think of it like having options for your home heating—each with pros and cons.
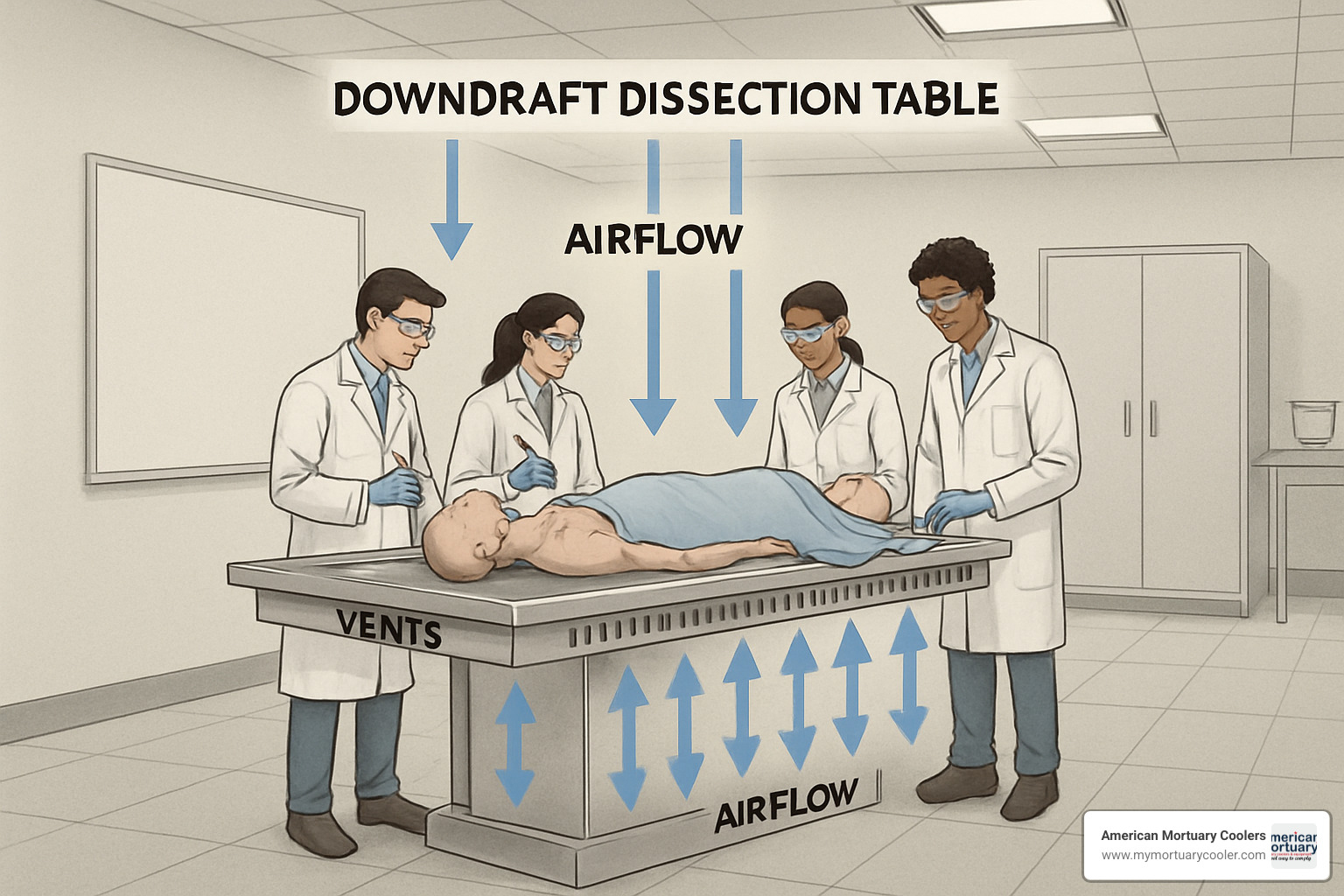
Downdraft tables are the premium option. They pull air downward through perforations in the table surface, capturing formaldehyde vapors right at the source before they can reach anyone's breathing zone. These systems are more energy-efficient since they target ventilation where it's needed most, but they come with a higher upfront cost. They're like having a kitchen hood that only turns on exactly where you're cooking.
Sidedraft tables take a different approach, capturing vapors horizontally at the table edges. They're excellent at containment but limit how you can arrange your lab. As one designer explained, "Sidedraft tables are like bowling lanes—they work great but you can't rearrange them for a dance party."
"Ballroom" style ventilation takes the simplest approach, using overall room air changes without specific capture points. This offers more flexibility for table arrangements but might require cranking up the total air changes to maintain safe conditions. It's less expensive to install but can cost more to operate over time.
The UC Riverside study put it well: "Ballroom style offers flexibility but may not guarantee formaldehyde limits without testing; sidedraft tables exceed containment requirements but at higher cost and fixed layout."
Smart labs are increasingly using Variable Air Volume (VAV) systems that adjust ventilation based on actual occupancy or even real-time contaminant levels. These systems can dial back to just 6-8 ACH during unoccupied hours, saving substantial energy while maintaining safety. Some labs are even integrating energy recovery systems that capture heat from exhaust air without risking cross-contamination.
Backup systems matter too. Redundant fans ensure negative pressure remains even during maintenance, and emergency power keeps ventilation running during outages. As one facility manager noted, "The chemicals don't care if the power's out—they'll still off-gas."
As ASHRAE guidelines emphasize, ventilation is just one piece of the safety puzzle. Personal protective equipment, good work practices, and administrative controls all work together with ventilation to create a safe learning environment.
Codes, Standards, and Safety Considerations Linked to Occupancy
When planning an anatomy lab, understanding the regulations that govern these spaces isn't just about checking boxes—it's about creating a safe environment where learning can thrive. The anatomy lab occupancy rate sits at the intersection of multiple safety codes that work together to protect everyone in the room.
Think of these regulations as the guardrails that keep anatomy labs safe while still being functional. They're not arbitrary rules, but rather the collective wisdom of safety experts who understand the unique challenges these spaces present.
The regulatory landscape includes several key frameworks that directly impact how many people can safely work in an anatomy lab:
NFPA 45 focuses on fire protection in chemical laboratories. While it no longer dictates specific air change rates (only requiring continuous ventilation), it does specify that any lab larger than 200 square feet containing hazardous materials needs two separate exits. This requirement directly connects to your anatomy lab occupancy rate since more people need more exit capacity.
OSHA's Laboratory Standard (29 CFR 1910.1450) requires every lab to have a Chemical Hygiene Plan and appropriate exposure controls. The more people in your lab, the more critical these controls become, as each person represents both a potential source of accidents and someone who needs protection.
ASHRAE 62.1 establishes the baseline ventilation standards that ensure acceptable indoor air quality. These minimums scale with occupancy, recognizing that more people generate more CO₂ and require more fresh air.
The ANSI Z358.1 standard requires emergency eyewash and shower equipment to be within a 10-second unobstructed walking distance from any spot in the lab. This "10-second rule" (about 55 feet of travel) becomes increasingly important as anatomy lab occupancy rates increase and workstations spread out.
State education authorities like SCHEV (State Council of Higher Education for Virginia) establish utilization benchmarks that influence how intensively spaces are used. Their guideline of 18 hours per week minimum utilization for class laboratories affects scheduling and, by extension, how many different groups will use the lab throughout the week.
Egress & Emergency Planning Based on Occupancy Load
When it comes to emergency planning, your anatomy lab occupancy rate isn't just a number—it's the foundation of your safety strategy. The more people in your lab, the more critical proper egress becomes.
Labs containing hazardous materials (which includes preservation chemicals) that exceed 200 square feet must have two separate ways out. These exit doors need to swing in the direction of travel—toward the exit, not into the lab—so people can quickly push through during an emergency without creating a bottleneck.
I once visited a university anatomy lab where storage cabinets had gradually encroached on the secondary exit path. While technically there were still two doors, one wasn't truly usable in an emergency. This highlights why keeping exit paths completely clear is non-negotiable, regardless of how tempting it is to use that space for storage.
Emergency equipment accessibility is equally important. Those eyewash and safety shower stations must be reachable within 10 seconds from anywhere someone might be working. When planning your lab layout, imagine a student or instructor with chemicals in their eyes—they need to reach that eyewash station quickly, even with impaired vision.
Fire extinguishers must remain visible and accessible at all times, and emergency power-off buttons should be positioned at every lab entrance for quick shutdown when needed.
As NC State University's Design Guidelines wisely point out, your secondary exit can't lead through another lab space. Each lab needs its own independent evacuation route to ensure one emergency doesn't trap people in adjacent areas.
Remember to plan for your maximum possible occupancy, not just your typical class size. Special events, combined classes, or observation days can push your numbers higher than normal, and your safety systems need to accommodate these peak loads.
Exposure Controls and Formaldehyde Compliance
Formaldehyde exposure control represents one of the most significant challenges in anatomy labs, and it's directly influenced by your anatomy lab occupancy rate. More people typically means more specimens are being worked with simultaneously, which can increase chemical concentrations in the air.
OSHA sets clear limits on formaldehyde exposure:
- 0.75 parts per million (ppm) averaged over an 8-hour workday
- 2 ppm maximum during any 15-minute period
- 0.5 ppm "action level" that triggers mandatory monitoring
Monitoring this exposure isn't a one-and-done task. Many labs use a combination of approaches: personal sampling badges worn by instructors and students, fixed monitoring stations throughout the room, and increasingly, real-time electronic sensors that can provide immediate feedback.
The relationship between people in the room and formaldehyde levels follows a predictable pattern: the concentration is proportional to the emission rate multiplied by the number of sources, divided by your ventilation rate. In simple terms, more cadavers and specimens (sources) require more air movement to maintain safe levels.
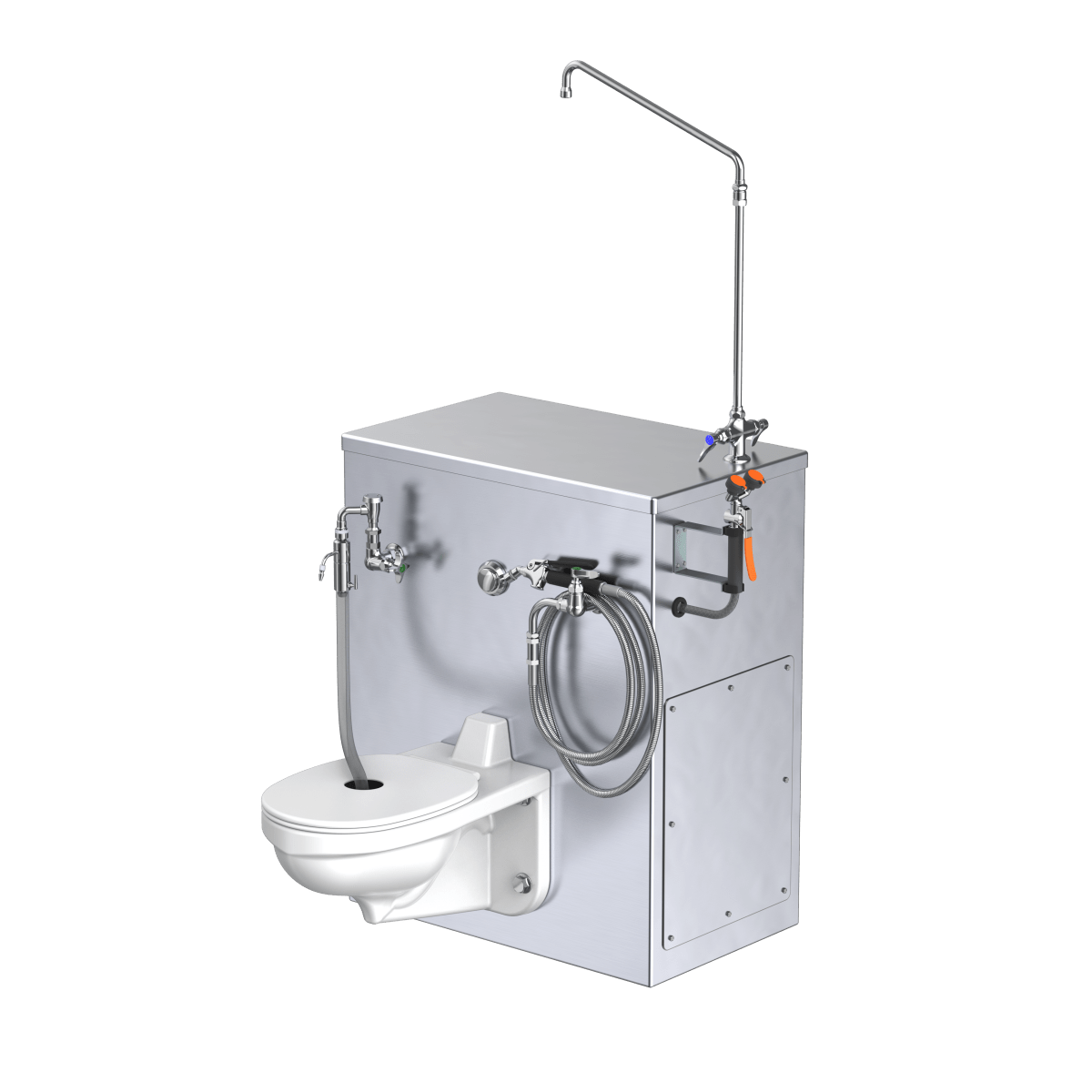
At American Mortuary Coolers, we've learned through years of experience that effective ventilation design must account for both the number of preserved specimens and the number of people working with them. Our Pathology Grossing Station solutions are built with this understanding, incorporating ventilation systems that maintain safe formaldehyde levels even as occupancy fluctuates throughout the day.
The best exposure control systems don't just meet minimum requirements—they adapt to changing conditions in real-time, ensuring everyone in the lab remains protected regardless of how many people are present or what activities are underway.
Monitoring, Optimization, and Future Best Practices

Remember the days when we'd just crank up the ventilation and hope for the best? Those days are thankfully behind us. Today's approach to managing anatomy lab occupancy rate is smarter, more responsive, and significantly more efficient.
Modern anatomy labs are becoming increasingly sophisticated in how they monitor both people and air quality. Walk into a cutting-edge facility and you might not notice the infrared beam counters at the doorway tracking entries and exits, or the discreet environmental sensors monitoring formaldehyde levels in real-time. These technologies aren't just cool gadgets – they're changing how we balance safety and sustainability.
"What gets measured gets managed," as the saying goes, and that's especially true for laboratory environments. Today's monitoring systems typically include occupancy counters (from simple infrared beams to privacy-filtered camera systems), environmental sensors that detect specific chemicals like formaldehyde, and utilization tracking through scheduling systems and access logs. Software platforms like LabStats can even track computer usage as another proxy for occupancy patterns.
The real magic happens when these systems talk to each other, creating a comprehensive picture of both real-time conditions and long-term patterns. This integration allows lab managers to make evidence-based decisions rather than relying on assumptions or worst-case scenarios.
Smart Sensors to Match Ventilation to Anatomy Lab Occupancy Rate
The days of one-size-fits-all ventilation are giving way to smarter, more responsive systems. Demand-based ventilation represents the cutting edge of laboratory management, using a network of sensors to dynamically adjust air flow based on actual conditions.
These smart systems typically use three types of monitoring: direct contaminant detection (sensors specifically calibrated for formaldehyde or broader VOC detection), occupancy monitoring (through motion sensors or using CO₂ as a proxy for human presence), and integrated monitoring networks that combine multiple sensor types for redundancy and comprehensive coverage.
I recently spoke with a laboratory manager at a medical school who implemented such a system. "It's like having a lab assistant who's constantly checking the air," she told me. "When students arrive for morning dissection, ventilation automatically ramps up. When they leave, it scales back. If someone opens a specimen container and releases formaldehyde, the system detects that spike and boosts air flow until levels normalize."
The research backs up this approach. Studies cited in comprehensive laboratory ventilation white papers suggest lab air is "clean" over 98% of the time under demand-based control. This finding opens the door to significant energy savings without compromising safety.
A well-designed system creates a continuous feedback loop that optimizes ventilation based on actual anatomy lab occupancy rate and environmental conditions:
- During nights and weekends: Maintain minimum ventilation (6-8 ACH)
- When people arrive: Increase to standard occupied rate (15 ACH)
- If chemical levels spike: Boost to maximum ventilation (20+ ACH)
- After air clears: Return to appropriate rate based on current occupancy
This responsiveness not only improves safety but dramatically reduces energy consumption – a win-win for both lab users and facility managers.
Energy & Cost Implications of High vs Low Occupancy
Let's talk dollars and sense. The energy consumption of anatomy labs is directly tied to ventilation rates, which in turn relate to occupancy patterns. Understanding this relationship reveals significant opportunities for savings.
Each additional air change per hour increases energy consumption by approximately 5-7%. When you consider that ventilation typically accounts for 60-70% of a laboratory's total energy use, those air changes add up quickly. The biggest energy drain comes from conditioning outside air – heating it in winter, cooling it in summer, and controlling humidity year-round.
The Yale University laboratory spill study found something fascinating: the greatest benefit in increasing air changes happens between 6 and 8 ACH, with minimal safety gains above 12 ACH. This suggests a smart approach – use higher ventilation rates when needed for occupancy or contamination events, but scale back during low-use periods.
Let me share a real-world example from a 2,000 square foot anatomy lab in a moderate climate:
A lab running constant high ventilation (20 ACH, 24/7) might face annual energy costs around $45,000. By simply implementing a schedule-based approach (20 ACH during typical 12-hour workdays, 8 ACH overnight), that same lab could save $12,000 annually. Taking it further with demand-based controls that vary between 6-20 ACH based on actual conditions could boost savings to $20,000 per year.
"We reduced our anatomy lab energy costs by over 30% with occupancy-based ventilation," one laboratory manager told me. "The system paid for itself in less than three years, and we've actually improved our formaldehyde exposure metrics because the system responds immediately to any detected releases."
At American Mortuary Coolers, we've seen this change firsthand. Our newer cooling systems are designed to interface with these smart building systems, adapting their operation based on both occupancy and environmental conditions. The integration creates safer, more efficient spaces that protect both people and budgets.
Frequently Asked Questions about Anatomy Lab Occupancy Rate
How many air changes per hour are required during unoccupied periods?
When everyone has left the anatomy lab for the day, you might wonder if all that powerful ventilation needs to keep running at full blast. The good news is that during unoccupied periods, you can typically reduce ventilation rates to just 6-8 air changes per hour (ACH), down from the 15-20 ACH needed when students are actively working with specimens.
This reduction still maintains basic air quality and keeps the negative pressure relationship with surrounding spaces, while giving your energy bill a much-needed break. The ASHRAE Laboratory Classification system provides some solid guidance here:
For LVDL-3 laboratories (most standard anatomy labs), a minimum of 6-8 ACH is recommended during unoccupied times, while the more hazardous LVDL-4 laboratories should maintain at least 8-10 ACH even when empty.
Before implementing these reductions, though, keep these important safety considerations in mind:
Always allow for a proper "purge period" (typically 30-60 minutes) after the last person leaves before reducing ventilation rates. Your monitoring systems should confirm that formaldehyde levels have dropped below action levels, and the system must be able to automatically ramp back up when someone enters. And of course, emergency override capabilities must remain functional at all times.
As one laboratory manager told me, "We save thousands in energy costs with our night setback program, but we never compromise on safety. The system automatically returns to full ventilation if anyone swipes into the lab after hours."
Can recirculated air ever be used in gross anatomy laboratories?
When it comes to recirculating air in anatomy lab settings, the short answer is: generally no, but there are some nuances worth understanding.
Most laboratory design standards take a firm stance on this issue. The NC State University Design Guidelines, for example, clearly state: "Recirculation of air is unacceptable in gross anatomy dissection labs; supply and exhaust ventilation must effectively remove airborne room contaminants in all room spaces to below allowable limits."
This makes perfect sense when you consider the hazards - formaldehyde and other preservatives need to be exhausted completely from the space, not just filtered and sent back in.
That said, there are a few limited scenarios where some form of recirculation might be acceptable:
Some facilities use sophisticated HEPA filtration combined with activated carbon or other chemical filtration to remove formaldehyde before recirculating a portion of the air. Energy recovery systems that transfer heating or cooling energy without actually mixing airstreams (like heat recovery wheels or run-around loops) can save energy without recirculating contaminants. And adjacent spaces that don't contain open specimens might allow some recirculation under certain conditions.
I've worked with several institutions that initially wanted recirculation systems to save energy, but ultimately decided the additional testing, monitoring and maintenance requirements weren't worth the potential risks. As one facility manager put it, "With something as critical as formaldehyde exposure, we prefer the certainty of 100% outside air."
What's the quickest way to verify if my lab exceeds its designed occupancy?
If you're wondering whether your anatomy lab occupancy rate exceeds safe limits, there are several practical ways to check without calling in consultants or engineers.
Start with the simplest calculation: measure your lab's net square footage (the actual usable floor space) and divide by 50 square feet per person, which is the NFPA standard. For example, a 1,500 square foot lab should accommodate no more than 30 people at once. This quick math gives you a good baseline.
Next, check the official building signage - most laboratories have maximum occupancy signs posted near entrances that indicate the legal limit established during permitting. This number should match or be more conservative than your calculation.
For a more operation-focused approach, count your dissection tables and multiply by the designed number of students per table (typically 4-6), then add instructors and teaching assistants. If your current class roster exceeds this number, you might be overcrowding the space.
While you're in the lab, take a moment to verify that you maintain proper clearances: 60 inches at the head and foot of each table, and 40-50 inches between tables. Make sure pathways to exits and emergency equipment remain completely unobstructed.
A lab manager at a medical school in the Midwest shared this practical tip: "We created a simple floor plan with colored zones showing the required clearances. During orientation, we show this to students so they understand why we're strict about keeping bags and coats in designated areas."
If any of these checks raise red flags, don't panic - but do consult with your institution's environmental health and safety department to develop a practical compliance plan. Your students' safety and education quality both depend on maintaining proper anatomy lab occupancy rates.
Conclusion
The journey through anatomy lab occupancy rate details has shown us that this isn't just a number on a building permit—it's the cornerstone of creating safe, effective learning environments for future medical professionals.
Throughout this guide, we've seen how the standard of 1 person per 50 net square feet isn't arbitrary. This spacing ensures students can move safely around dissection tables, quickly reach emergency equipment if needed, and work in an environment with proper ventilation. It's about creating a space where learning can happen without compromise.
Speaking of ventilation, we've learned that anatomy labs need robust systems providing 15-20 air changes per hour when students and faculty are present. But there's room for smart management too—reducing to 6-8 ACH during off-hours can save significant energy without sacrificing safety. This kind of thoughtful approach to lab management reflects what we at American Mortuary Coolers have seen work well in practice.
The regulatory landscape might seem complex, with NFPA, OSHA, and ASHRAE requirements creating what can feel like a maze of compliance. But there's wisdom in these overlapping standards—they form a safety net that protects everyone in these specialized environments.
One of the most exciting findings we've discussed is how strategic management of occupancy and ventilation schedules can cut energy use by 20-30% while maintaining safety standards. The Yale spill study confirms what many lab managers have finded through experience: smart management pays dividends in both safety and savings.
Looking ahead, we're seeing more labs accept intelligent systems—sensors that detect actual conditions, controls that respond in real-time, and monitoring that provides peace of mind. These technologies aren't just bells and whistles; they're changing how we think about laboratory safety and efficiency.
At American Mortuary Coolers, we've spent years helping design environments where preservation, safety, and education intersect. We've seen how thoughtful planning around occupancy and ventilation creates better educational spaces—places where the next generation of healthcare professionals can learn with confidence.
For those planning new anatomy labs or updating existing facilities, we encourage a risk-informed approach. Look beyond minimum requirements to consider your specific educational goals, how your space will actually be used day-to-day, and your institution's energy efficiency targets.
To learn more about our complete range of solutions for anatomy laboratories and related facilities, visit our information page or reach out to our design team directly.
Understanding and properly managing your anatomy lab occupancy rate isn't just about compliance—it's about creating an environment where learning thrives and safety is never compromised. It's about honoring the gift of those who donated their bodies to science by ensuring their contribution supports the best possible education in the safest possible setting.