The Life-Saving Journey of Organ Donation
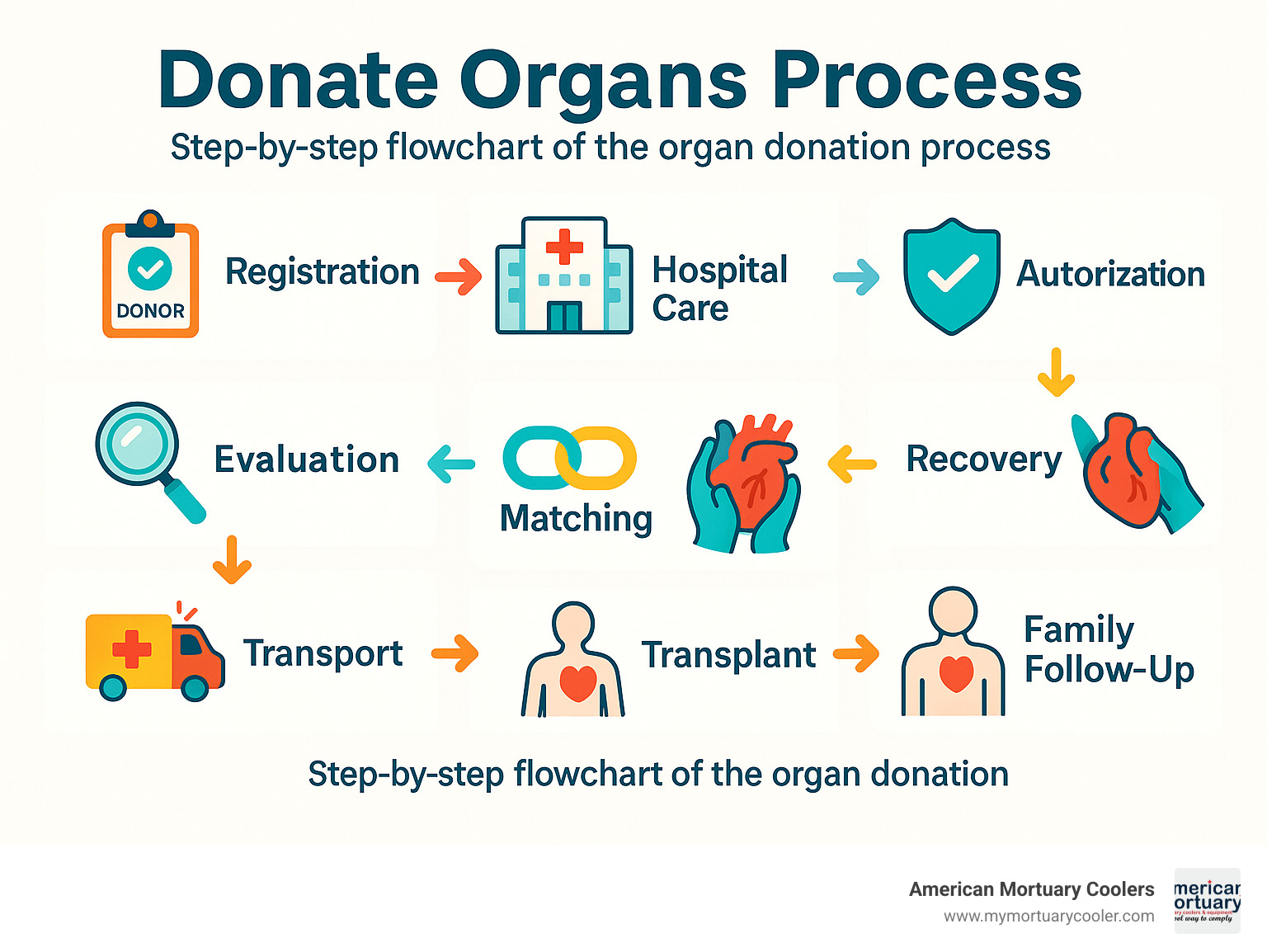
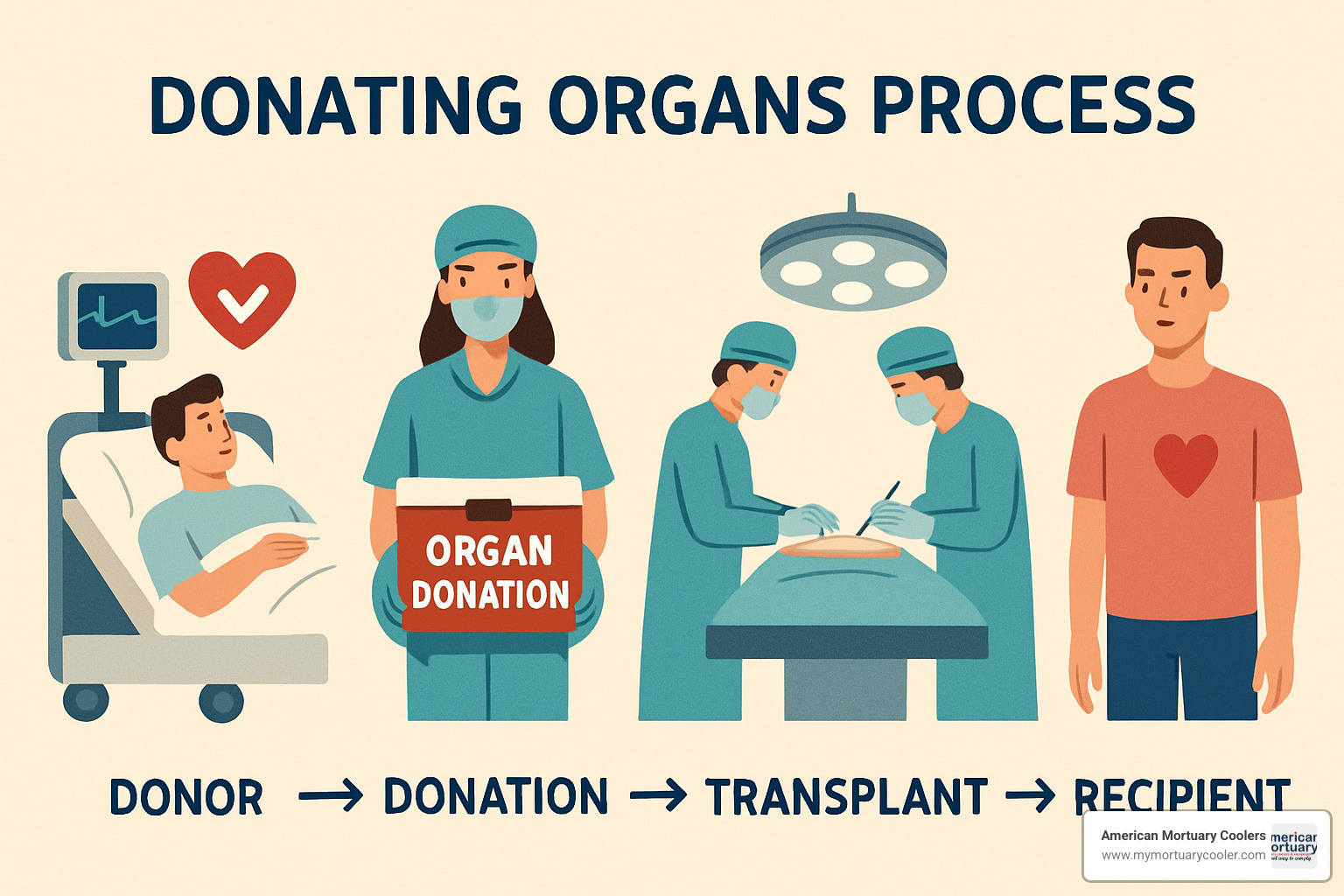
The donating organs process is a structured medical procedure that allows organs from one person to be transplanted into another to save lives. Here's a quick overview:
- Registration: Person registers as an organ donor through state DMV, online registry, or health app
- Medical Emergency: If registered donor suffers brain death or cardiac death
- Referral: Hospital contacts Organ Procurement Organization (OPO)
- Evaluation: Medical suitability is determined through tests
- Authorization: Registry status confirmed or family gives consent
- Matching: UNOS computer system matches organs to recipients
- Recovery: Surgical teams carefully remove donated organs
- Transport: Organs transported to recipient hospitals
- Transplant: Recipients receive life-saving organs
- Follow-up: Donor families receive information about transplant outcomes
Every day across America, over 100,000 people wait for life-saving organ transplants, with a new person added every 8 minutes. Despite 170 million registered donors, only about 3 in 1,000 people who die become actual organ donors due to specific medical criteria.
The donating organs process involves complex coordination between hospitals, organ procurement organizations, and transplant centers to ensure both respect for the donor and the best possible outcomes for recipients.
"Organ donation offers a second chance at life," according to transplant specialists, who note that a single donor can save up to 8 lives through organ donation and heal more than 75 people through tissue donation.
Understanding Organ Donation & Transplantation
The gift of life through organ donation is one of medicine's most remarkable achievements. When we talk about the donating organs process, we're describing something both simple and complex: taking a healthy organ from one person and giving it to someone whose own organ has failed.
There are two main paths to donation:
Deceased donation occurs after someone has passed away, either after brain death (when all brain function has irreversibly stopped) or after cardiac death (when the heart stops beating permanently).
Living donation is when someone who's alive chooses to donate an organ or part of an organ while they continue their own life journey.
The donating organs process operates under careful regulation through the National Organ Transplant Act of 1984, creating a nationwide network ensuring organs are shared fairly and ethically.
Why Organ Donation Matters
The impact of organ donation extends far beyond what most people realize:
- One organ donor can save up to 8 lives through their generosity
- The same donor can heal more than 75 people through tissue donation
- Every 8 minutes, another person joins the national transplant waiting list
- Organ donation builds bridges between communities that might otherwise never connect
As one recipient expressed, "My donor didn't just give me an organ; they gave me my future, my children's mother back, and my husband's wife."
What Organs & Tissues Can Be Donated After Death
When someone becomes a deceased donor, their final act of generosity can take many forms:
- Heart: Can beat in someone else's chest, giving them years they wouldn't otherwise have
- Lungs: Can help someone with cystic fibrosis breathe freely again
- Liver: Has an amazing ability to regenerate and can help two different recipients
- Kidneys: The most commonly transplanted organs, can free two people from dialysis
- Pancreas: Can give a diabetic patient freedom from insulin injections
- Intestines: Can save someone suffering from intestinal failure
- Tissues: Corneas restore sight, skin helps burn victims, bone replaces what's lost to trauma
Time is always of the essence in the donating organs process. Hearts and lungs must reach recipients within 4-6 hours, livers within 12-18 hours, and kidneys within 24-48 hours.
What Can Be Donated While Alive
Living donors offer something extraordinary – a piece of themselves to save another:
- Most commonly, people donate one kidney, as we can live healthy lives with just one
- Some brave donors give a liver lobe, knowing both pieces will regenerate within months
- Less frequently, living donors may give a lung lobe or intestine segment
- Others regularly donate bone marrow and stem cells or blood and platelets
Comparing Post-Mortem vs. Living Donations:
| Factor | Deceased Donation | Living Donation |
|---|---|---|
| Organs available | All major organs + tissues | Primarily kidney and liver |
| Wait time for recipient | Months to years | Scheduled in advance |
| Donor evaluation | Post-mortem | Extensive pre-screening |
| Recovery for donor | N/A | 6-12 weeks (kidney), 8-12 weeks (liver) |
| Organ function | Good | Excellent |
| Graft survival | Good | Better long-term outcomes |

To learn more about the remarkable benefits of organ donation, the Cleveland Clinic offers excellent scientific research on how many lives can be saved.
The Donating Organs Process Step-by-Step
When someone becomes an organ donor, they set in motion a life-saving chain of events. The donating organs process involves careful coordination between multiple teams working with one goal: giving someone else a second chance at life.
First comes the referral. When a patient faces end-of-life circumstances, hospitals are legally required to contact their regional Organ Procurement Organization (OPO).
Next, the OPO evaluation begins. Coordinators determine if organ donation is medically possible through blood tests, medical images, and patient history review.
The family authorization step is handled with sensitivity. If the patient is already registered as a donor, this serves as legal authorization. If not, OPO specialists have a compassionate conversation with the family.
Once consent is secured, the UNOS matching process begins. The donor's medical information enters the United Network for Organ Sharing system, which generates a prioritized list of potential recipients based on medical criteria.
Then comes the surgical recovery, where specialized teams carefully recover the donated organs with the same precision and respect as any lifesaving surgery.
The preservation and transport phase is where timing becomes critical. Each organ has its own viability window:
- Heart/Lungs: 4-6 hours
- Liver: 12-18 hours
- Pancreas: 8-12 hours
- Intestine: ~8 hours
- Kidneys: 24-48 hours
Finally, transplantation occurs as recipients undergo surgery to receive their new organs, while the donor's body is prepared with the utmost care for funeral arrangements.
Donating Organs Process in Deceased Donation
There are two main pathways for deceased donation:
With Donation after Brain Death (DBD), the patient remains on a ventilator in the ICU, keeping organs supplied with oxygen-rich blood. Brain death is confirmed through multiple rigorous tests performed by physicians not involved in transplantation. Once brain death is declared, the person is legally deceased, though their heart continues beating with ventilator support until organ recovery.
The second pathway is Donation after Cardiac Death (DCD). This option is for patients with severe injuries who don't meet brain death criteria but have no chance of recovery. After the family decides to withdraw life support, death is declared once the heart stops beating. Organs must be recovered quickly after cardiac death, making timing especially critical.
Matching Donors to Recipients
The matching process is managed through UNOS's national computer system called UNet. Finding the right recipient involves multiple factors:
- Blood type compatibility is non-negotiable
- Tissue typing (HLA) looks at genetic markers that influence acceptance
- Body size matters tremendously, especially for heart and lung transplants
- Medical urgency often takes priority
- Time on the waiting list helps ensure fairness
- Geographic distance affects transport time and organ viability
The system is deliberately blind to factors like race, wealth, celebrity status, or connections, ensuring allocation remains equitable and transparent.
Funeral & Body Care After Donation
One common concern is whether donation affects funeral plans. Open-casket viewings and funerals are absolutely possible after organ donation.
The surgical teams use careful techniques that preserve the body's external appearance. Incisions are made discreetly and closed with the same care as in any surgery. The donor is treated with profound respect throughout the entire process.
After organ recovery, the donor's body is carefully prepared and transported to the family's chosen funeral home. Both cremation and burial options remain completely available – donation doesn't limit these choices in any way.
Living Donation: Options, Eligibility, Risks
Living donation allows you to share the gift of life while you're still here to witness the difference you've made. There are several ways to become a living donor:
Directed Donation is the most common path, where you donate directly to someone you know and love, dramatically reducing their waiting time.
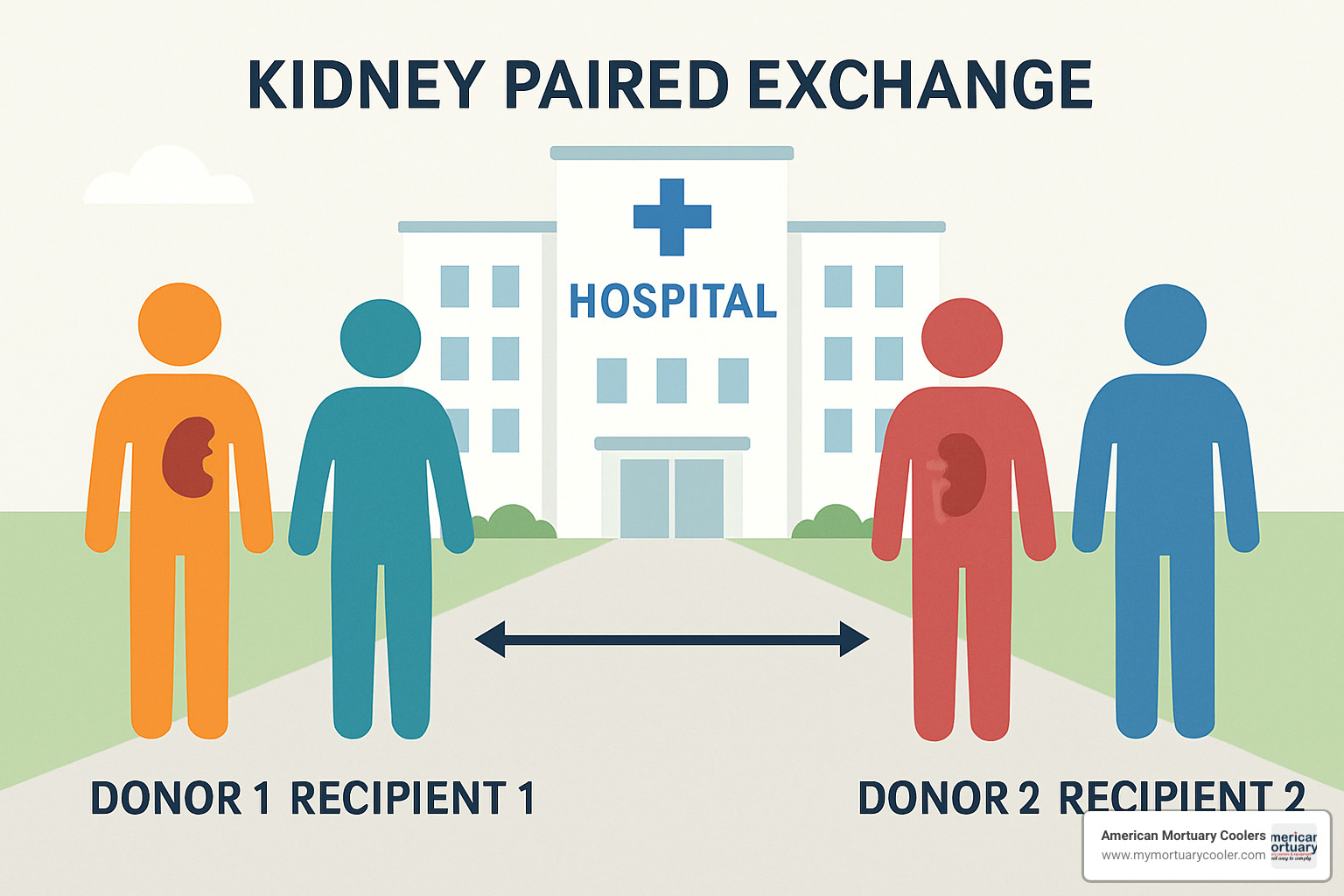
Paired Kidney Exchange works like a matchmaking service. If you're incompatible with your intended recipient, you can be matched with another incompatible pair. You donate to their recipient, while their donor gives to your loved one.
Donation Chains often begin with an altruistic donor and can facilitate dozens of transplants in a domino effect. Some chains have included more than 30 transplants.
Non-directed (Altruistic) Donation is giving an organ to whoever needs it most on the waiting list, someone you've never met.
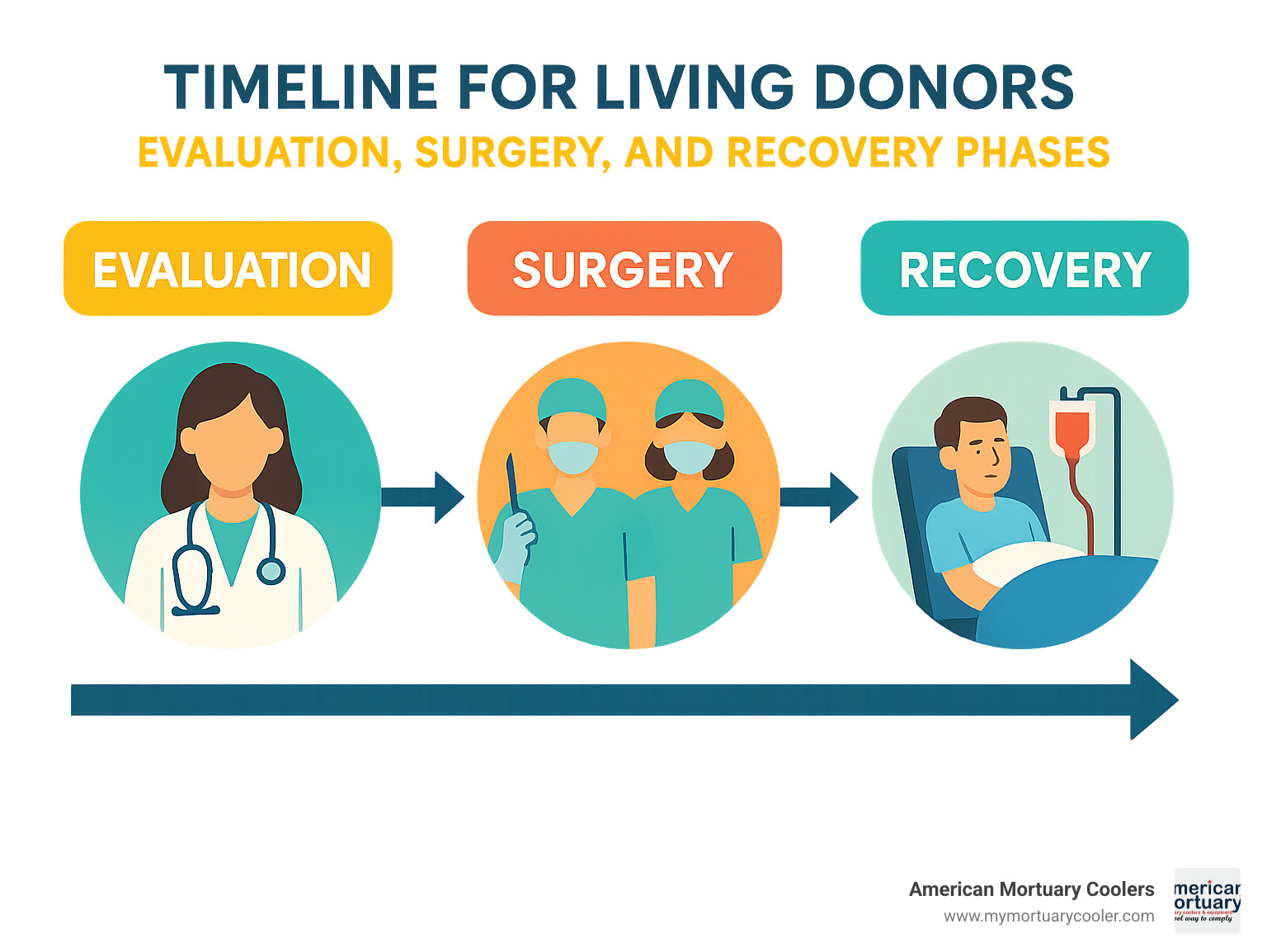
The evaluation process typically takes 3-6 months and includes comprehensive medical testing, psychological evaluation, financial consultation, and meetings with an independent advocate who represents only your interests.
Eligibility & Evaluation for Living Donors
Most centers look for donors between 18-65 years old in good physical and mental health, without uncontrolled conditions like high blood pressure, diabetes, cancer, HIV, hepatitis, or kidney disease. A BMI under 35 is typically preferred.
The evaluation process usually begins with an initial screening questionnaire and blood tests to check basic compatibility. If you pass this stage, you'll move on to a more comprehensive medical evaluation including a physical exam, detailed lab work, and imaging studies.
A psychosocial assessment helps ensure you're emotionally prepared for donation. You'll also meet with an independent donor advocate and have a financial consultation to understand potential costs and assistance options.
Risks & Recovery Timeline
Living donation carries certain risks, including infection, bleeding, blood clots, adverse reactions to anesthesia, and pain. The risk of death is very low but real – approximately 1 in 3,000 for kidney donors and 1 in 500 for liver donors.
Kidney donors can live normal, healthy lives with one kidney, which grows slightly to compensate. Liver donors experience remarkable regeneration, with their liver growing back to nearly full size within 2-3 months.
Long-term, kidney donors may have a slightly increased risk of high blood pressure or reduced kidney function later in life. However, studies show that the psychological benefits often far outweigh these risks.
Recovery varies by donation type. Kidney donors typically stay in the hospital for 2-3 days and return to work within 2-6 weeks. Liver donors usually spend 5-7 days in the hospital and need 8-12 weeks before returning to work.
Financial & Legal Considerations for Living Donors
While selling organs is illegal in the United States, donors should be aware of potential financial impacts, which might include travel expenses, lodging, lost wages, and childcare expenses.
Fortunately, several assistance options exist. The National Living Donor Assistance Center (NLDAC) provides grants for qualifying donors. The recipient's insurance typically covers the donor's medical expenses related to evaluation, surgery, and follow-up care.
Legal protections include the Family and Medical Leave Act (FMLA), which provides job protection for eligible employees. Some states have enacted additional job protections specifically for living donors.
Myths, Costs & Support Resources
Let's clear up some common misconceptions about organ donation that keep many people from registering.
Common Myths vs Facts About the Donating Organs Process
"I'm too old to donate" - There's no age cutoff for organ donation. What matters is the condition of your organs, not your birthday. The oldest organ donor on record was 92 years old!
"Being a donor might affect my medical care" - This concern couldn't be further from the truth. The medical teams working to save your life are completely separate from transplant teams. The donating organs process only begins after all life-saving efforts have been exhausted.
"My religion prohibits donation" - Nearly all major religions view organ donation as an act of charity and compassion.
"I can't have an open-casket funeral" - You absolutely can have an open-casket funeral after organ donation. The recovery surgery is performed with the same care and respect as any other medical procedure.
"Wealth and fame move you up the transplant list" - The organ matching system doesn't care about your bank account or status. Medical urgency, blood type compatibility, and time on the waiting list determine who receives organs.
Financial Questions Answered
For donor families, there is absolutely zero cost associated with organ donation. Your family will never see a bill for any part of the donating organs process.
For transplant recipients, most insurance plans, Medicare, and Medicaid cover transplant surgeries. Transplant centers have dedicated financial coordinators to help with insurance and identify assistance programs.
Living donors face different considerations. While the recipient's insurance typically covers medical expenses related to donation, there can be indirect costs like travel and lost wages. The National Living Donor Assistance Center offers grants to help with these expenses.
Support for Donor Families & Recipients
Organ Procurement Organizations provide bereavement support and counseling referrals for donor families. Families receive follow-up letters explaining which organs were transplanted, offering comfort in knowing their loved one's gifts are helping others.
Many families find healing through annual memorial events and support groups. When both parties consent, correspondence between donor families and recipients can provide profound comfort.
Transplant recipients receive support through transplant centers' support groups, counseling, and mentorship programs connecting new recipients with those further along in recovery.
For more information about morgue coolers that support the donation process, visit our guide to morgue coolers.
How to Register & Take Action Today
Becoming an organ donor is one of the most meaningful decisions you can make—and it's surprisingly simple. You can register through several convenient methods:
State Driver's License/ID: Check the donor box when getting or renewing your license at your local DMV.
National Donate Life Registry: Visit RegisterMe.org to join the national registry in just a few minutes.
iPhone Health App: Apple users can register directly through the Medical ID feature in their Health app.
State Registry: Each state maintains its own donor registry with slightly different processes.
Perhaps the most crucial step after registering is sharing your decision with your family. While your registration is legally binding in most states, having this conversation brings clarity and comfort during what would already be a challenging time.
Step-by-Step Guide to Sign Up
The donating organs process begins with your registration, which takes just minutes:
Choose your preferred registration method—whether online, at the DMV, or through a health app.
Complete a simple form with basic information like your name, date of birth, and address.
Some registries allow you to specify donation preferences, though most donors choose to donate all viable organs and tissues.
After you submit your registration, you'll receive confirmation—keep this for your records.
Update your emergency contacts about your decision.
Consider including your donation wishes in your advance directive or living will.
You can modify or withdraw your consent at any time by contacting your state registry.
Starting the Donating Organs Process as a Living Donor
If you're considering becoming a living donor, the journey begins with these steps:
Contact the transplant center where your intended recipient is registered, or any transplant center for non-directed donation.
Complete an initial screening questionnaire and blood tests to determine basic compatibility.
Meet with the living donor team, including surgeons, nephrologists, psychologists, and social workers.
If initial screening is favorable, begin a comprehensive medical evaluation.
Meet with an independent living donor advocate who represents only your interests.
With all information in hand, make an informed decision.
If approved and you choose to proceed, schedule surgery.
Conclusion & Industry Perspective
The donating organs process represents one of humanity's most beautiful expressions of generosity. A single decision to become a donor can create ripples of hope, healing dozens of lives. Throughout this article, we've explored this remarkable journey—a carefully orchestrated process that brings medical teams, grieving families, and grateful recipients together in a profound circle of life.
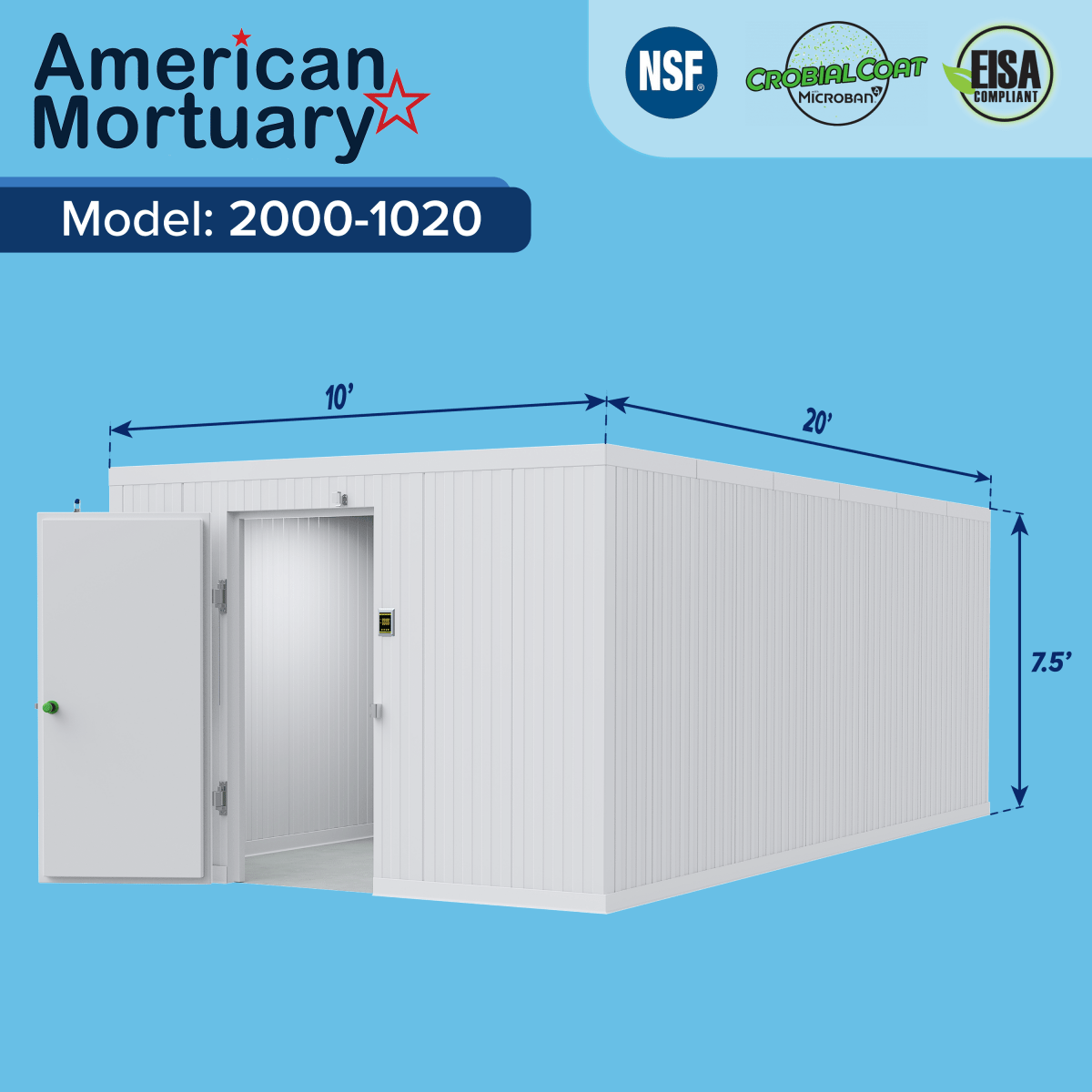
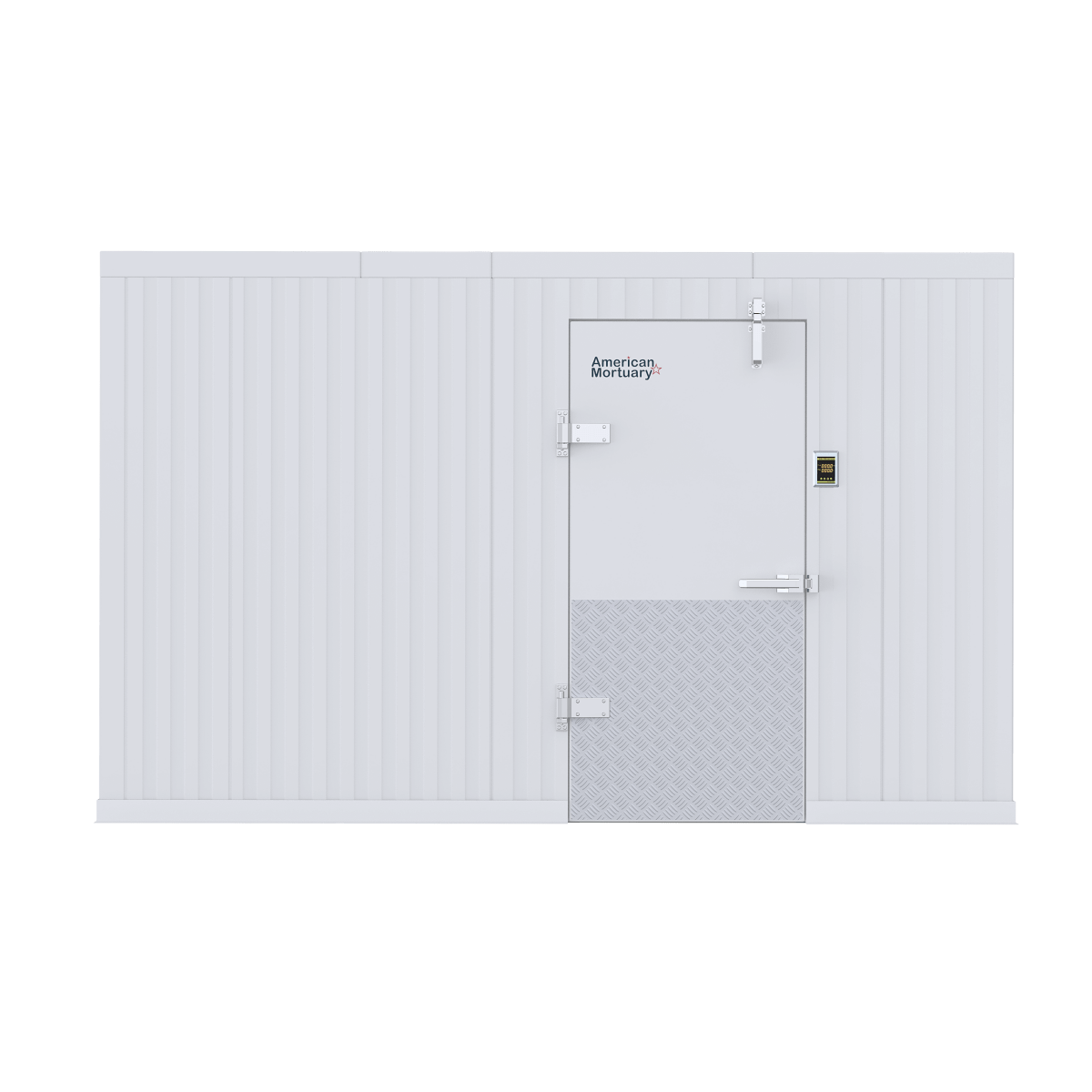
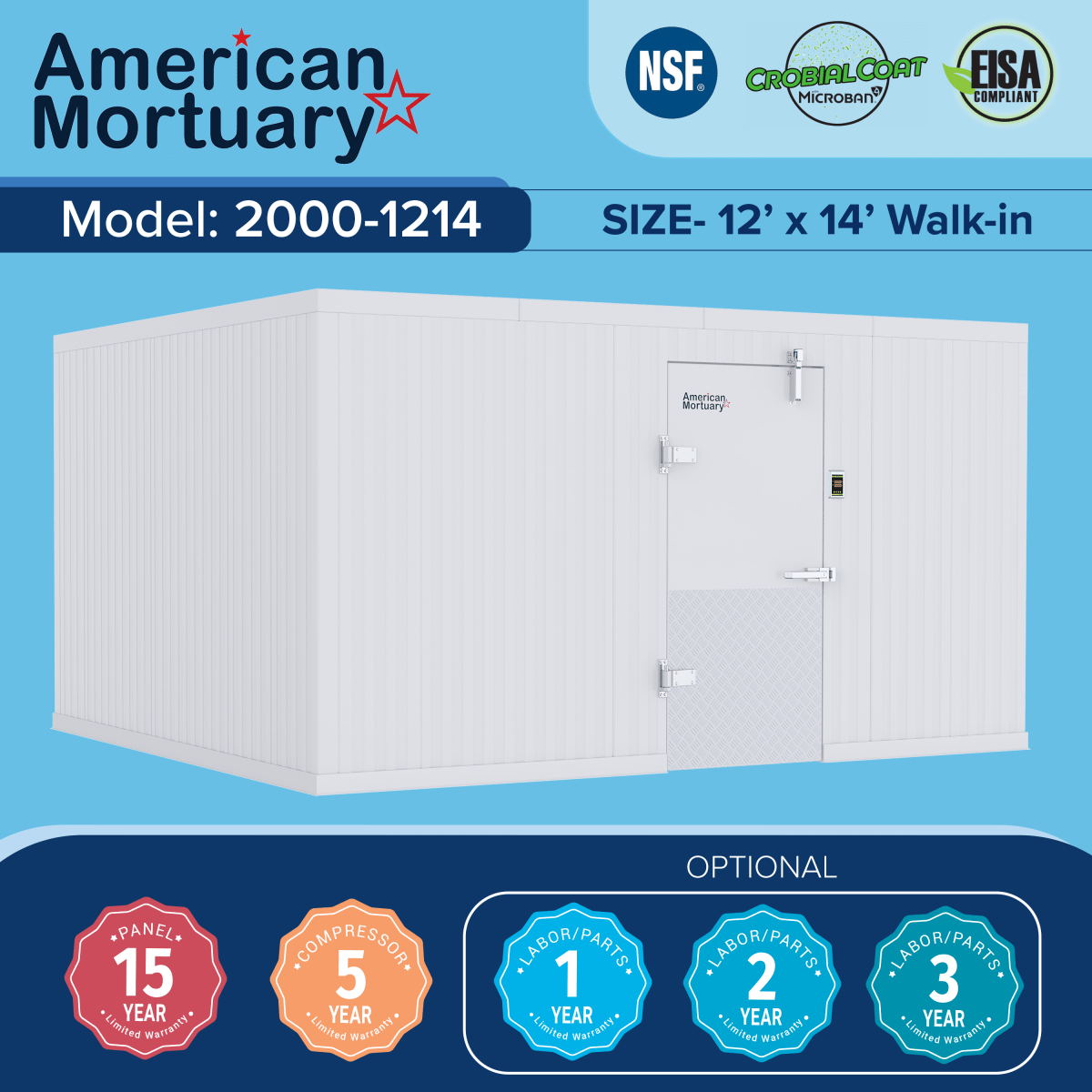
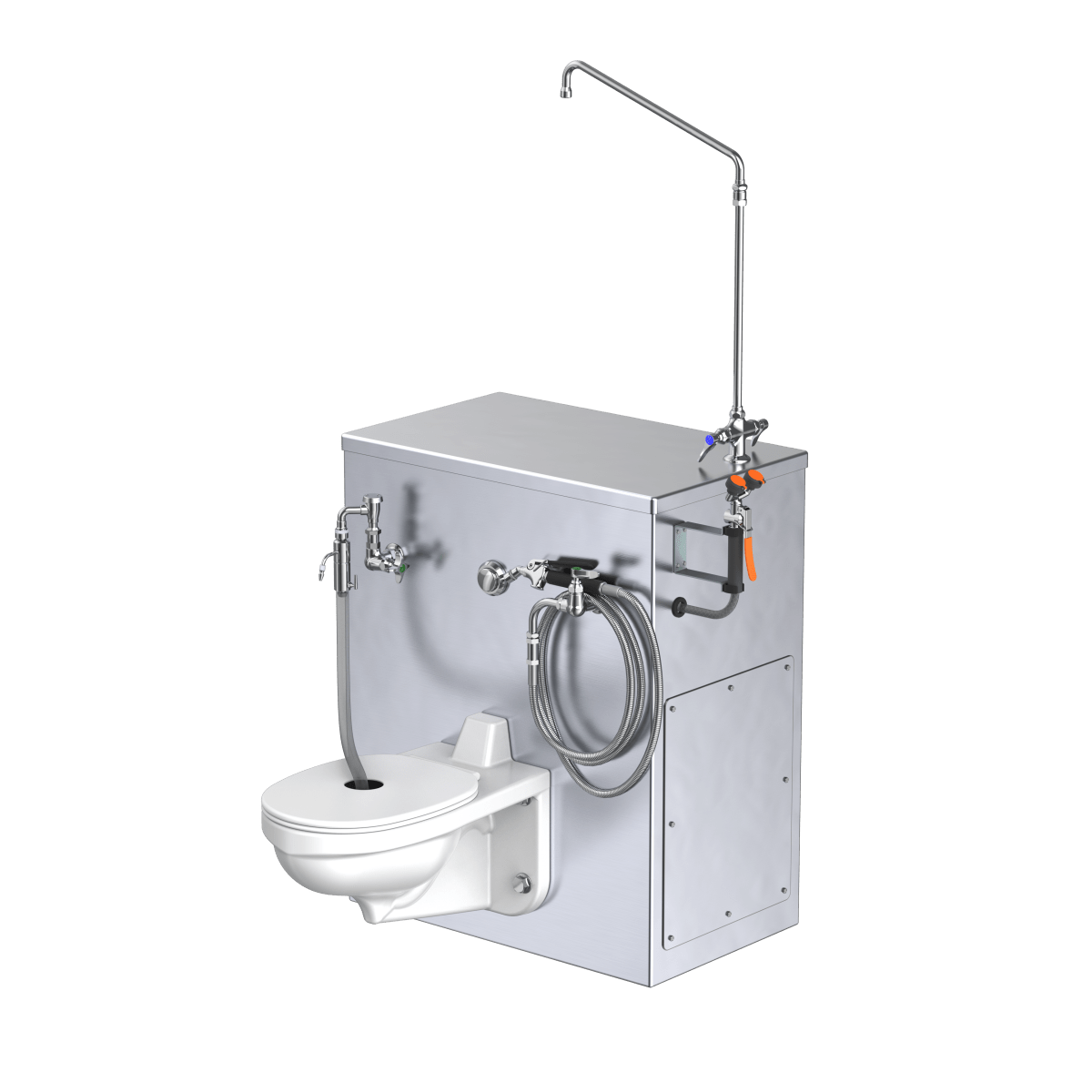
At American Mortuary Coolers, we're privileged to play our role in this life-saving process. Based in Tennessee with locations throughout the country, our team crafts custom mortuary coolers and refrigeration solutions that help maintain the dignity of donors after they've given their final gift. We deliver our durable, thoughtfully designed equipment directly to funeral homes, hospitals, and medical examiner facilities across the lower 48 states.
Proper preservation after organ recovery allows families to proceed with meaningful funeral rituals. Many families find comfort in open-casket viewings, and our specialized equipment ensures these wishes can be honored. Every donor deserves to be treated with the utmost respect, and we're committed to supporting that mission through every piece of equipment we build.
The gap between need and availability remains significant—over 100,000 Americans wait each day for a transplant that could save their life. But together, we can help close this gap. Whether you're considering registering as a deceased donor, exploring living donation options, or simply seeking to understand the process better, I hope this guide has illuminated the remarkable journey of organ donation.
If you work in the funeral industry and need reliable mortuary refrigeration solutions that support the donating organs process, please visit our website or reach out to our team in Johnson City, TN, or any of our regional offices across the country.
I encourage you to join the 170 million Americans who have already registered as organ donors. Your decision today could give someone else the chance at tomorrow.