Understanding Emergency Childbirth: When Babies Don't Wait
What is emergency delivery? An emergency delivery occurs when a baby is born unexpectedly outside of a planned healthcare setting, without medical professionals present or with minimal preparation time. This can happen in homes, vehicles, or other non-hospital locations when labor progresses too rapidly to reach medical care.
| Emergency Delivery Overview |
|---|
| Definition: Precipitous birth in an unexpected setting without planned healthcare support |
| Incidence: Approximately 0.61% of all U.S. births |
| Common Settings: Homes, vehicles, emergency departments |
| Warning Signs: Contractions <5 minutes apart, overwhelming urge to push, bulging perineum |
| Key Actions: Call 911, prepare clean area, support baby's head during delivery, keep baby warm |
Every year, nearly 9,000 women in the United States go into labor and, unable to make it to the hospital, have an unplanned or unattended birth. These situations represent a small but significant portion of births that require immediate action to ensure the safety of both mother and baby.
Emergency deliveries often occur with mothers who have given birth before or who experience "precipitous labor" - labor that progresses extremely rapidly, sometimes in less than 3 hours from start to finish.
"Despite what you may see on TV, emergency homebirths aren't common—only about one in 250 babies arrives suddenly. Although frightening, women are designed to birth babies and your body knows what to do," notes one expert source.
When facing an emergency delivery, staying calm is crucial. Most emergency births proceed normally without complications, but knowing the basics can make a significant difference in outcomes.

What is Emergency Delivery?
What is emergency delivery in simple terms? It's when a baby decides to arrive unexpectedly - often quickly and dramatically - outside of a planned medical setting. Medical professionals call these situations "born-before-arrival" or BBA births, and they happen when labor progresses so rapidly that there's simply no time to reach the hospital, birthing center, or for a midwife to arrive for a planned home birth.
Though relatively rare, these unexpected arrivals make up about 0.61% of all U.S. births. That small percentage translates to thousands of babies each year making their grand entrance in homes, cars, public places, or even in hospital emergency departments before the mother can be transferred to the labor and delivery unit.

Despite the dramatic circumstances, it's reassuring to remember that human bodies are designed for childbirth. As one labor and delivery nurse who ended up delivering her own baby on Interstate 30 wisely noted, "Although this kind of thing happens on sitcoms, not to seasoned labor and delivery nurses, your body knows what to do."
For a deeper understanding of the medical research on this topic, you might want to review scientific research on unplanned out-of-hospital births.
How Common and Where It Happens
Emergency deliveries can happen virtually anywhere, though some settings are more common than others.
Home settings account for about one in 250 births in Australia that occur suddenly, with similar rates in other developed countries. These unplanned home births most commonly happen to women who've given birth before and experienced fast labors previously.
Vehicles become delivery rooms more often than you might think! Cars, taxis, and other transportation frequently become birthplaces when parents are racing to the hospital.
Ambulances sometimes become mobile delivery rooms after emergency services have been called but before reaching the hospital. While paramedics and EMTs receive training in basic delivery techniques, they may not have specialized obstetric equipment on board.
Emergency departments handle a subset of imminent deliveries despite most hospital births occurring under obstetric care.
The frequency of emergency births varies around the world. In the United States, about 0.61% of all births occur in unplanned settings. California reported 1.34% of births taking place outside hospitals in 2020, though most of these were actually planned home births.
Recognizing and Preparing for an Imminent Emergency Birth
When a baby decides it's time to arrive, sometimes they don't wait for the hospital! Recognizing the signs that birth is imminent can make all the difference between panic and preparedness.
Your body gives clear signals when birth is approaching quickly. Strong, regular contractions occurring less than 5 minutes apart and lasting nearly a minute each are a major clue. When your water breaks with that unmistakable gush or steady trickle of fluid, things are definitely progressing. Perhaps the most telling sign is an overwhelming urge to push – this powerful, involuntary sensation feels remarkably like needing to have a bowel movement and shouldn't be ignored.
You might also notice intense rectal pressure as baby's head enters the birth canal, along with bloody show (pink or blood-tinged mucus). When the perineum begins to bulge and stretch, delivery is very close. The most definitive sign is crowning – when you can actually see the baby's head at the vaginal opening.
"I thought I had hours left, but when I felt that unstoppable urge to push, I knew we weren't making it to the hospital," shares one mom who delivered in her bathroom. "My body just took over."
True labor and Braxton-Hicks contractions can sometimes be confusing. Here's how to tell them apart:
| True Labor | False Labor (Braxton-Hicks) |
|---|---|
| Contractions get stronger, longer, and closer together | Contractions remain irregular and don't intensify |
| Pain usually starts in back and radiates to abdomen | Discomfort mainly in abdomen |
| Walking makes contractions stronger | Walking may relieve contractions |
| Cervix progressively dilates and effaces | No cervical changes |
| Bloody show may be present | No bloody show |
Essential Supplies and Setup
Creating a safe space for an unexpected birth doesn't require hospital-grade equipment, just some basic supplies and common sense. For your emergency birth kit, gather sterile gloves (several pairs if possible), clean towels and blankets to dry and warm baby, and something to clamp and cut the cord. In a pinch, shoelaces, clean string, or dental floss can work as cord clamps.
Also helpful: sterile scissors (or a very clean knife), a bulb syringe for clearing baby's airways, plastic sheets to create a clean surface, hand sanitizer, a small hat for baby, and sanitary pads for postpartum bleeding.
When setting up your impromptu birthing area, find the cleanest possible location and wash your hands thoroughly. Create a clean surface with plastic sheets and towels, and keep the room warm – at least 72°F is ideal for newborns.
When to Call 911 or Transfer
Call 911 immediately when:
Water breaks with heavy bleeding or the fluid is green/brown (indicating possible meconium), contractions are less than 5 minutes apart and intensifying, there's an overwhelming urge to push, or any part of the baby is visible. Also call if the mother feels the baby is coming right now, experiences severe, constant abdominal pain, shows signs of high blood pressure (severe headache, vision changes), or has any known high-risk condition.
When talking to emergency dispatchers, be clear and concise: provide your exact location, explain that birth appears imminent, mention how far along the pregnancy is (especially if less than 37 weeks), describe any visible parts of the baby, and report any complications. Most importantly, stay on the line – dispatchers can provide invaluable guidance while help is on the way.
Performing an Emergency Delivery: Step-by-Step Guide
When a baby decides it's time to make an entrance and help hasn't arrived yet, knowing what to do can make all the difference. Let's walk through this together, step by step:
First, help mom get comfortable. A semi-sitting position with knees bent and legs apart often works best. If she's alone, lying down or sitting propped up against something sturdy is safest.
Before you do anything else, wash your hands thoroughly or use hand sanitizer. If you have gloves available, put them on.
As the baby's head begins to crown (becomes visible at the vaginal opening), gently support the perineum with a clean towel. This gentle counter-pressure helps control the delivery and reduces tearing.
When the head emerges, support it gently with your hands. Remember: never pull on the baby. Let gravity and mom's contractions do the work. The head should deliver slowly, ideally between contractions.
Once the head is out, check if the umbilical cord is wrapped around the baby's neck (called a nuchal cord). If it is:
- Try to gently slip it over the baby's head
- If it's too tight, try to loosen it enough to allow delivery
After the head delivers, it will naturally turn to one side. With the next contraction, guide the baby's head gently downward to deliver the upper shoulder, then upward for the lower shoulder.
The rest of the baby usually slides out quickly after the shoulders. Support the baby's body as it emerges, and be careful—newborns are surprisingly slippery!
If possible, wait 30-60 seconds before clamping and cutting the cord. This brief delay allows more blood to transfer from the placenta to the baby.
Stages of Labor in an Emergency Context
Understanding where mom is in the labor process helps you know what to expect next:
Stage 1: Dilation and Effacement of the Cervix This is when the cervix opens and thins. In emergency situations, this stage may be lightning-fast, especially for women who've given birth before. Contractions start 5-30 minutes apart during early labor and get closer together as labor progresses.
Stage 2: Expulsion (Pushing and Birth) This is the main event! It begins when the cervix is fully dilated (10 cm) and ends with baby's birth. For first-time moms, this averages about 36 minutes, while experienced moms might push for just 6-12 minutes.
Stage 3: Delivery of the Placenta Within 5-30 minutes after birth, mom will deliver the placenta (afterbirth). You'll notice a small gush of blood, the umbilical cord lengthening, and mom feeling another urge to push.
Immediate Newborn Actions
Once your little one has arrived, these first moments are crucial:
Note the time of birth. A healthy newborn should start breathing and crying within seconds.
Gently wipe the baby's face, nose, and mouth with a clean cloth. Avoid deep suctioning which can actually cause a dangerously slow heart rate.
Quickly dry the baby with clean towels and place them skin-to-skin on mom's chest. Cover both with dry blankets, keeping baby's face visible. This skin-to-skin contact is nature's perfect incubator—it regulates baby's temperature, heart rate, and breathing.
If the baby isn't breathing well, stimulate them by continuing to dry vigorously, rubbing the back, or gently flicking the soles of the feet. If there's no response after 30 seconds, begin rescue breathing.
Help the baby latch onto the breast when possible. Early breastfeeding stabilizes baby's temperature and blood sugar, releases oxytocin (which helps the uterus contract and reduces bleeding), and begins the bonding process.
Navigating Complications on the Fly
While most emergency deliveries go smoothly, complications can arise when you least expect them. Knowing how to handle these situations could mean the difference between a good outcome and a crisis.
Breech Presentation
When a baby decides to come feet or bottom first instead of head first, stay calm. This is a breech presentation, and while challenging, you can handle it.
Don't pull on the baby's body – this is absolutely crucial. Nature needs to take its course here. Allow the body to deliver naturally up to the belly button (umbilicus). If the head doesn't deliver within 3-5 minutes after the body emerges:
- Help mom get into a hands-and-knees position if possible
- Gently support the baby's body, letting it hang down naturally
- Create an airway by placing two fingers in a "V" shape on either side of the baby's nose
- Call for emergency help immediately – this is not the time to go it alone
Shoulder Dystocia
Sometimes a baby's head delivers smoothly, but then everything stops – the shoulders get stuck behind mom's pubic bone. This is shoulder dystocia, and it requires quick action.
Remember the HELPERR approach:
H: Call for Help – you'll need it E: Evaluate for episiotomy (rarely needed in emergency settings) L: Legs (McRoberts maneuver) – sharply flex mom's legs against her abdomen P: Suprapubic Pressure – have someone apply firm pressure just above mom's pubic bone E: Enter maneuvers – internal rotation techniques (for medical professionals) R: Roll mom onto hands and knees – this often frees the stuck shoulder R: Remove the posterior arm (for medical professionals)
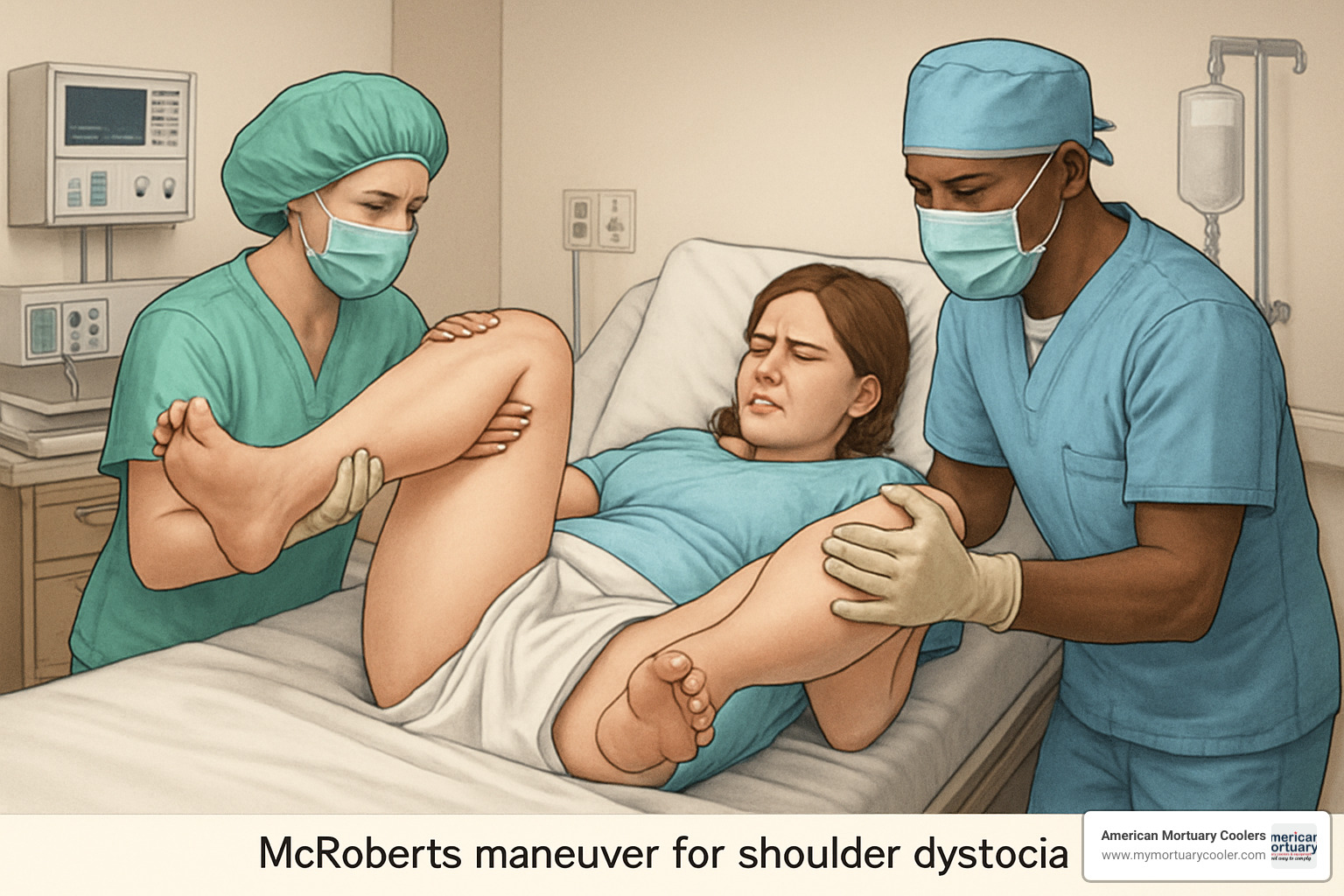
The McRoberts maneuver is your first go-to move and surprisingly effective. By sharply flexing mom's legs against her abdomen, you can straighten her pelvis and create more room for the baby's shoulders to slip through.
Umbilical Cord Prolapse
If you see the umbilical cord come out before the baby, this is an emergency situation requiring immediate action. The cord is baby's lifeline, and if it gets compressed, oxygen supply is cut off.
Get mom into a knee-chest position or extreme head-down position immediately. Then, with a clean, gloved hand, gently push the presenting part (usually the head) off the cord to relieve pressure. Keep your hand in place until help arrives.
Never try to push the cord back in. Instead, keep it moist with clean towels if possible. Continue monitoring for pulsations in the cord, which tell you baby is still getting blood flow.
Postpartum Hemorrhage
Excessive bleeding after delivery (more than 500 mL – about two cups) is a postpartum hemorrhage. Most of the time (70-80%), this happens because the uterus isn't contracting properly.
Your first and most important step is to massage the uterus firmly. Place one hand just above mom's pubic bone and the other on her abdomen, then massage firmly but gently. This helps the uterus contract and close off bleeding blood vessels.
Encourage breastfeeding or nipple stimulation – this releases oxytocin, nature's way of making the uterus contract. Have mom empty her bladder if possible, as a full bladder can prevent proper uterine contractions.
Post-Delivery Care, Follow-Up & FAQs
After an emergency delivery, taking proper care of both mother and baby is crucial until professional help arrives. Those first moments can be overwhelming, but with a few simple steps, you can help ensure everyone stays safe and comfortable.
For the Mother:
Keeping a close eye on mom is essential after delivery. Check her pulse and breathing every 15 minutes to make sure she's stable. One of the most important things you can do is perform gentle fundal massage - this means softly massaging the top of the uterus through the abdomen every 15 minutes to help it contract and prevent excessive bleeding.
Some bleeding is completely normal after birth - typically less than 500 mL (about 2 cups). More than this could indicate a problem. Keep mom warm with blankets to prevent shock, and offer water or clear fluids if available to keep her hydrated.
The placenta usually delivers within 30 minutes after the baby. Don't pull on the umbilical cord to try to speed this process! When it does deliver, save it for medical inspection.
For the Baby:
Skin-to-skin contact works wonders for newborns. Place the baby directly on the mother's chest, covering both with dry blankets while leaving the baby's face visible. This natural approach helps regulate the baby's temperature, breathing, and blood sugar levels.
Keep a close eye on the baby's breathing - newborns typically take 40-60 breaths per minute. Their breathing might look a bit irregular at first, which is normal.

Transfer to Hospital:
Even if everything seems perfect with both mother and baby, medical evaluation is essential as soon as possible. The mother needs assessment for tears, retained placental fragments, and other postpartum complications. The baby needs a complete newborn examination, weight check, and possibly vitamin K injection to prevent bleeding problems.
Frequently Asked Questions about What is Emergency Delivery
Q: What if I feel the urge to push but help hasn't arrived?
A: That overwhelming urge to push can be powerful! If you can't resist it, try panting in short breaths instead of holding your breath and pushing hard. Find a comfortable position - semi-sitting or side-lying often works well. Support your perineum with a clean towel if possible.
Let your body guide you rather than forcing the push. When a contraction comes, push gently if you need to, and remember to breathe between pushes. Your body knows what to do - trust it!
Q: Is it safe to cut the umbilical cord in an emergency?
A: Ideally, wait for medical professionals to arrive before cutting the cord. If that's not possible, wait until the cord stops pulsating (usually 1-3 minutes) - this ensures your baby gets all those beneficial nutrients and blood cells.
If you must cut it, tie it tightly in two places, about 2 inches apart, at least 6 inches from the baby. Use sterilized scissors or a clean knife to cut between the ties.
Q: What if the placenta doesn't deliver within 30 minutes?
A: If the placenta doesn't deliver within half an hour, don't panic - and definitely don't pull on the cord! Try gentle nipple stimulation or breastfeeding, which releases oxytocin to help the uterus contract. Having mom empty her bladder can sometimes help too.
Q: How do I know if bleeding is excessive after delivery?
A: While some bleeding is normal after childbirth, it's excessive if it soaks more than one pad per hour or if mom passes large clots bigger than a plum. Other warning signs include dizziness, faintness, or a rapid pulse.
Conclusion
Emergency deliveries might sound like something from a dramatic TV show, but they're real-life events that require quick thinking and calm action. While uncommon, being prepared with knowledge can make all the difference when a baby decides it's time to arrive – ready or not!
Throughout this guide, we've explored what is emergency delivery and how to handle this unexpected situation with confidence. The good news? Your body knows what it's doing, even when your birth plan takes an unexpected turn.
Remember these essential takeaways:
Most emergency births proceed normally without complications. The human body has been bringing babies into the world long before hospitals existed. Trust in this natural process while taking sensible precautions.
Staying calm is your superpower in this situation. Deep breaths help you think clearly and respond effectively to what's happening. Your calmness will also help the laboring mother feel more secure during an intense experience.
Focus on the basics: keep mother and baby warm (skin-to-skin contact works wonders), manage any bleeding through gentle uterine massage, and ensure the baby is breathing well. These simple actions address the most critical needs until help arrives.
Even after a seemingly perfect emergency delivery, professional medical evaluation is essential. Hidden complications can develop hours after birth, so don't skip this important step.
At American Mortuary Coolers, we understand emergency preparedness from our work providing specialized equipment to healthcare facilities across the country. From our Tennessee headquarters, we've seen how preparation and quick thinking make all the difference in critical situations.
For more information about our specialized mortuary equipment solutions that support healthcare facilities nationwide, visit our mortuary coolers solutions page.